Trismus or limited mouth opening is a major complication of oral cancer. Radiation therapy is crucial in treating oral cancer, but in the long run, it leads to fibrosis, trismus and muscular stiffness that restricts oral functions. In advanced cases, Trismus Correction surgery is the only option. Other options available for treatment are the release of fibres and reconstruction using local flaps.
Nasolabial Flap
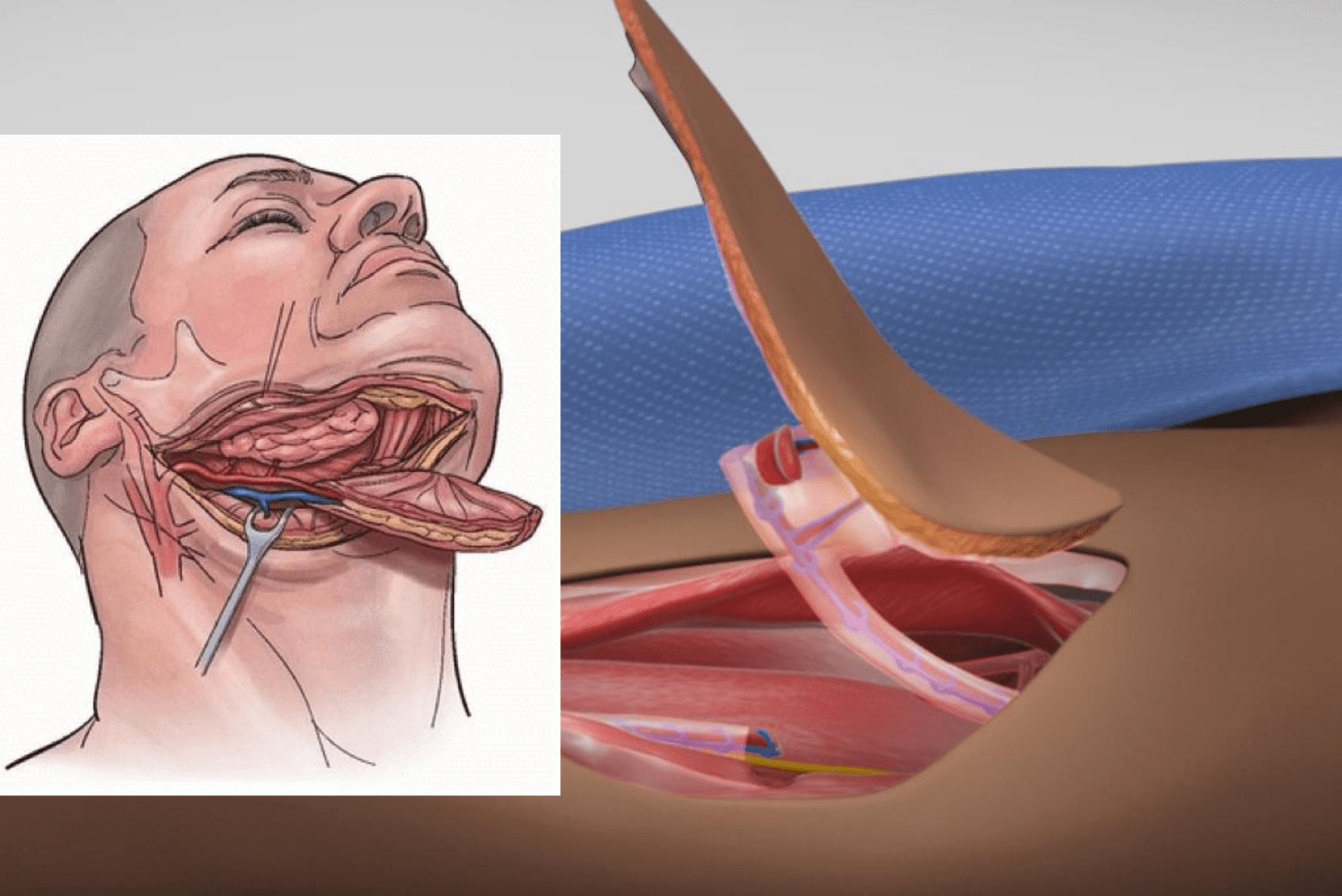
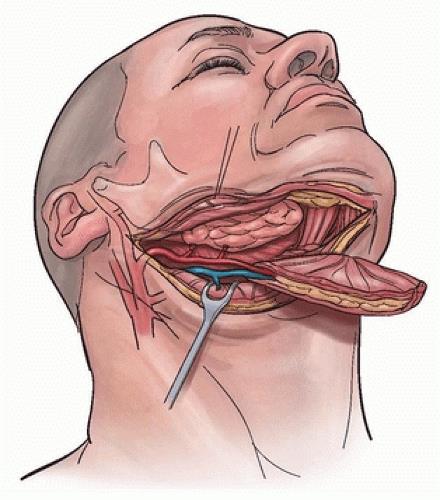
This flap is taken from the tissue along the sides of your nose and cheek region. A fair amount of spindle-shaped flap can be taken for closure of defects created inside the mouth after fibrotomy. Fibrotomy is a procedure where the fibrous bands restricting the mouth opening after radiation therapy are excised. After this, the space between the muscles has to be filled with a healthy muscle that can keep the buccal mucosa supple enough to aid in mouth opening. This procedure is often part of trismus correction post-radiation therapy.
The nasolabial flap is a simple flap used for reconstructing small intraoral defects created after the excision of malignant tumours. Results in a good overall cosmetic and functional outcome. Several methods described for reconstructing oral defects use either pedicled or free flaps. The pectoralis major flap, a pedicled flap, is commonly used for this purpose; however, this flap is bulky and is associated with considerable donor site morbidity. Likewise, the radial forearm free flap has also become a preferable reconstruction method. It offers a large surface of thin, pliable skin that allows for complex reconstruction, but unfortunately, donor site morbidity rates are quite high, for example, through delayed wound healing and exposure of tendons. The need for microsurgical expertise is a major disadvantage. This makes nasolabial flaps ideal for the reconstruction of small intraoral defects and is widely used in trismus correction post-radiation therapy.
The nasolabial flap is a very simple flap used for reconstruction of intraoral defects in the floor of the mouth, the tongue, cheek, commissures, nose tip, nasal ala, and lower eyelids. It is a preferred technique for trismus correction post-radiation therapy due to its minimal donor site morbidity and effective functional restoration.
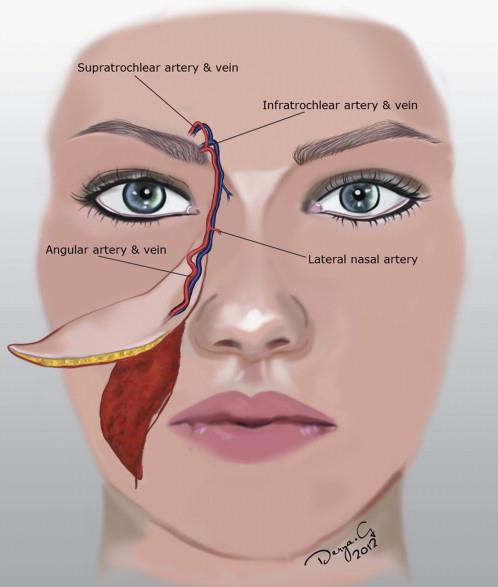
The nasolabial flap may be superiorly or inferiorly based. An inferiorly based flap is useful in reconstruction of the lip, oral commissure, and anterior aspect of the floor of the mouth, while superiorly based flaps are utilised for reconstruction of the ala and tip of the nose, and the lower eyelids and cheeks. This technique is highly effective in trismus correction post-radiation therapy.
Intraoral reconstruction with a nasolabial flap is a simple and fast procedure with minimal donor defect and complications, making it a preferred choice for trismus correction post-radiation therapy.
Submental Flap
The submental flap provides an alternative technique in orofacial reconstruction, especially in situations where free flap services are not available. This flap is highly useful in trismus correction post-radiation therapy.
The reconstruction of orofacial defects after an ablative tumour surgery has both functional and morphological impacts. Reconstruction using microvascular free flaps is the gold standard but requires a high degree of expertise, cost, time consumption, and prolonged hospital stay. The last three decades have witnessed a paradigm shift in the field of microvascular free flap reconstruction for orofacial defects. The submental flap offers a reliable option for trismus correction post-radiation therapy.
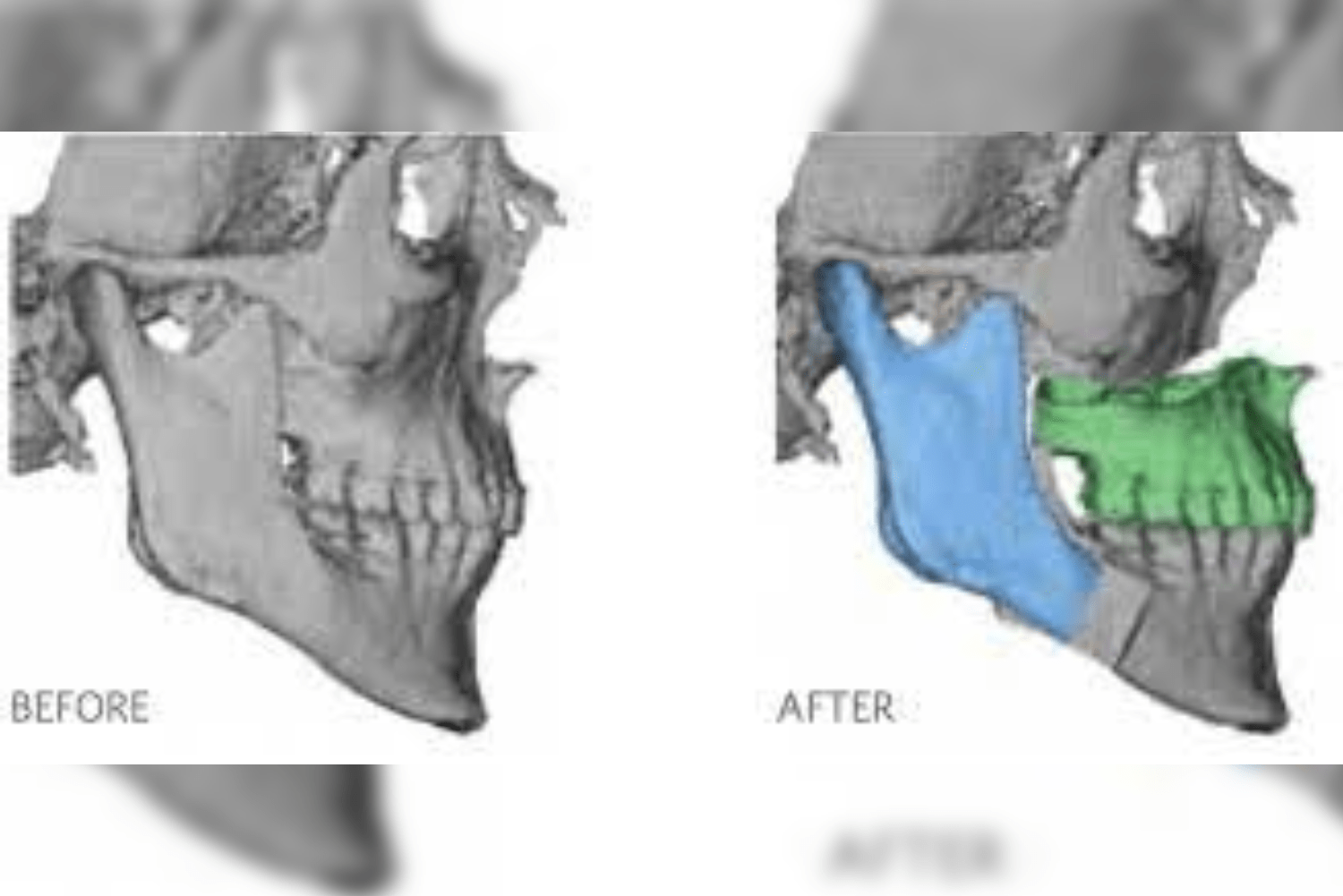
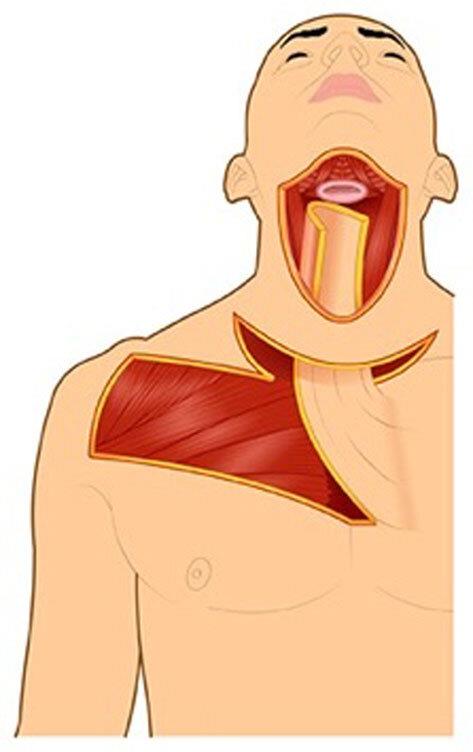
Submental artery island flap was first described by Martin et al. in 1993 in their attempt to search for an alternate to free flap while matching colour, shape, and tissue texture. It has a long (up to 8 cm), consistent, reliable pedicle, and cutaneous dimensions reaching up to 7 cm × 18 cm. It can be used as a cutaneous, musculofascial (cervicofacial and platysma), or osteocutaneous flap. The flap has an excellent skin colour match, a wide arc of rotation, and can extend to the whole homolateral face and oral cavity, making it highly effective in trismus correction post-radiation therapy.
Over the last 2 decades, it has become popular as a reliable choice in the reconstruction of oral cavity defects and in trismus correction post-radiation therapy. It is an axial pattern skin flap based on the submental artery, a consistent branch of the facial artery.
The submental island flap has shown promising results due to its versatile use, wide arc of rotation, excellent color match, low donor site morbidity, and effectiveness in trismus correction post-radiation therapy.
Deltopectoral Flap
The deltopectoral (DP) flap represents a reconstructive option for the head and neck and can be effectively used in trismus correction post-radiation therapy. It is a skin and muscle flap raised from the anterior chest wall below the clavicle. Its role partially declined with the rise of free flaps. However, it still remains a valid option in patients who cannot undergo reconstruction with free flaps. It is known for its reliable anatomy, good colour matching with the facial skin, and texture. It is easily handled by a surgeon with lower failure rates.
Key aspects of the deltopectoral flap:
Anatomy:
The flap has its blood supply from an artery present in the chest region near the clavicle. It is the internal mammary artery, typically the second to fourth intercostal perforators. The flap consists of skin and subcutaneous tissue from the chest and shoulder area, extending towards the midline dividing our body. It is commonly used in trismus correction post-radiation therapy for reconstructive purposes.
Indications:
It is used to reconstruct defects in the head and neck, those caused by tumour removal or fistulas (abnormal connections) or defects after trismus release, particularly in trismus correction post-radiation therapy. Specifically, it is used for:
-
Reconstruction of the cheek, oral cavity, pharynx, and neck
-
Covering exposed vessels or fistulas in the neck
-
Serving as a “backup” flap for failed free flaps or other reconstructive procedures
Advantages:
-
Reliable: The flap has a predictable anatomy and blood supply.
-
Good Colour Match: The skin of the flap often provides a good colour and texture match with the facial skin.
-
Ease of Harvesting: It can be harvested relatively quickly and easily.
-
Can be Delayed: This flap can be harvested in stages to increase its length and reach.
-
Can be Returned: The pedicle (blood supply) can be divided and returned to the donor site after a period of time, minimizing donor site morbidity, which is particularly helpful in trismus correction post-radiation therapy.
Disadvantages:
-
Donor Site Scarring: The donor site defect may sometimes be large enough to require a skin graft, potentially resulting in noticeable scarring.
-
Potential for Necrosis: In longer flaps, distal flap necrosis can occur. Patients with diabetes mellitus have a higher risk of postoperative necrosis of the distal portion of the flap.
-
Hairy Skin: In some patients, the flap may include hairy skin, leading to hair growth in the oral cavity or on the face, which can be undesirable in certain reconstructive situations, including trismus correction post-radiation therapy.
Surgical Technique:
-
The flap is outlined on the chest and shoulder region, including the deltopectoral groove.
-
Skin and subcutaneous tissue are elevated while carefully preserving the blood vessels.
-
The flap is then rotated or transposed to the recipient site.
-
The donor site is covered and sutured, often with a skin graft, to ensure proper healing and functionality, especially in cases like trismus correction post-radiation therapy.
Modern Considerations:The DP flap offers versatility in head and neck reconstruction. Depending on the tissue volume needed, the distance from the donor site, and patient-specific factors, this flap can be adapted to achieve optimal functional and aesthetic outcomes, particularly in trismus correction post-radiation therapy.
Anterolateral Thigh Flap
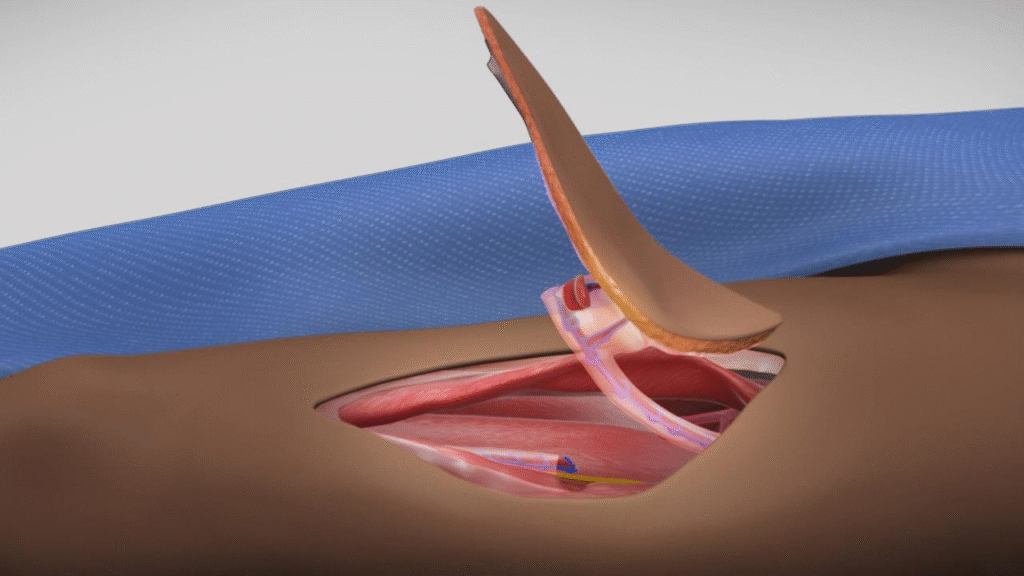
To cover the defects created on the face, a patch of skin, along with the fat and sometimes even muscle, from the front and outer part of your thigh is taken to replace the missing tissue elsewhere. The anterolateral thigh (ALT) flap allows for healthy, reliable, vascularized, soft-tissue coverage of defects of traumatic or acquired deformities. It can be used to cover defects created after trismus correction post-radiation therapy or mandible resection to aid in mouth opening.
The ALT flap was described by Song et al., which is based on blood supply emanating from the descending branch of the lateral femoral circumflex artery, which is present in the thigh region.
The magic behind the ALT flap lies in its blood supply. Your skin, muscles, and tissues are supplied by the network of blood vessels called perforators. One such perforator that supplies blood to this flap lies in the thigh and is a branch of the lateral femoral circumflex artery.
Why the Thigh?
The anterolateral thigh is a popular choice for trismus correction post-radiation therapy reconstruction because:
-
Lots of Tissue: A generous amount of tissue is available, including skin and bulky muscle for reconstruction.
-
Versatility: The flap is versatile, suitable for both small and large defects. It can be thinned down or harvested in bulk depending on defect size.
-
Long Blood Vessels: The donor perforator has a long length, aiding in easy microvascular attachment with the recipient vessel.
-
Hidden Scar: The scar at the donor site is well hidden on the side of the thigh, making it inconspicuous.
-
Minimal Impact on the Thigh: Raising the flap generally doesn’t affect thigh muscle function, minimizing morbidity.