Craniofacial anomalies are the most complex congenital deformities in humans. It not only impacts the appearance but also vital functions like breathing, eating and speaking. Amongst these anomalies Tessier clefts represent a rare subset of facial clefts.
They are considered to be complex beyond the more familiar cleft of lip and palate. Paul Tessier in 1970 described this class that are more challenging amongst the most experienced craniofacial surgeons and requires a comprehensive and multidisciplinary approach for effective management.
Let us explore in depth about Tessier clefts and their treatment.
What are Tessier clefts?
A Tessier cleft or craniofacial clefts are rare congenital facial anomalies that result from the disruption in the normal fusion of facial structures during embryonic development. Unlike the most common cleft lip and cleft palate, these clefts affect other facial structures involving both soft and hard tissues. A French pioneer craniofacial surgeon called Paul Tessier introduced a classification system for these clefts in 1976 that is still widely used today. These clefts are named after him as Tessier clefts.
Tessier classification system
A systematic method to classify facial clefts was developed by Tessier based on their anatomical location on the face. This system assigns numbers 0 to 14 to the clefts based on their anatomical location. 0–7 represents facial clefts extending from the midline towards the outer regions of the face. 8 to 14 represents cranial clefts extending from the facial cleft into the cranial bones.
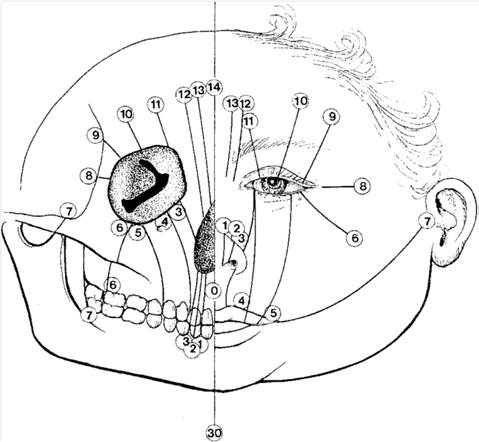
Each cleft is present bilaterally, creating pairs like 0 & 14 and 1 & 13, with the orbit acting as the centre of this clock-like diagram.
Facial Clefts (0–7):
-
0: Midline cleft of the upper lip (median cleft lip)
-
1–2: Paramedian clefts (involving lip, maxilla, and nasal septum)
-
3: Naso-ocular cleft
-
4: Infraorbital cleft
-
5–7: Lateral clefts (toward the zygoma and ear)
Cranial Clefts (8–14):
These are the superior extensions of the facial clefts. 8–14 mirror clefts 6–0 respectively, involving the orbit, forehead, and sometimes the brain.
This system allows for more precise surgical planning and multidisciplinary communication.
Etiology
The face develops between the fourth and 10th gestational weeks from the fusion of facial prominences. There are five facial prominences: one frontonasal, two maxillary and two mandibular. These prominences come together and fuse in the midline to form the face. Any disturbance in their fusion or the formation of bone will lead to a cleft between the bones and the muscle/skin covering it. These are identified as clefts.
Reasons for these clefts include:
-
Genetic Mutations
-
Vascular Disruption
-
Exposure to Alcohol
-
Certain Medications during pregnancy
-
Unknown multifactorial causes
Unlike the typical cleft lip and palate, there is a high level of tissue breakdown after fusion in Tessier clefts, which is why their appearance is varied and severe.
Clinical presentation
The clinical appearance and severity of Tessier clefts vary widely depending on the location and the clefts involved. Some of the most notable features are:
Soft tissue deformities-facial symmetry duplicated or missing anatomical structures, wide set of eyes or hypertelorism, coloboma or eyelid notches.

Bony abnormalities-missing or malformed Maxilla zygomatic bone orbits nasal bones and or or frontal bone.

Functional impairment-problem with vision, eating, breathing, hearing, or speaking.
Neurological abnormality like if the cleft extends into the cranium brain anomaly such as NFO seal may be present.
Each cleft number has specific characteristic features for example :
Tessier 0 has midline cleft clip nose duplication and possible brain analysis. Tessier 3 features a cleft involving the upper lip nasal and the lower lid.
Testier 7 involves macrostomia or a widened mouth along with hemifacial microsomia.
Diagnosis and Imaging
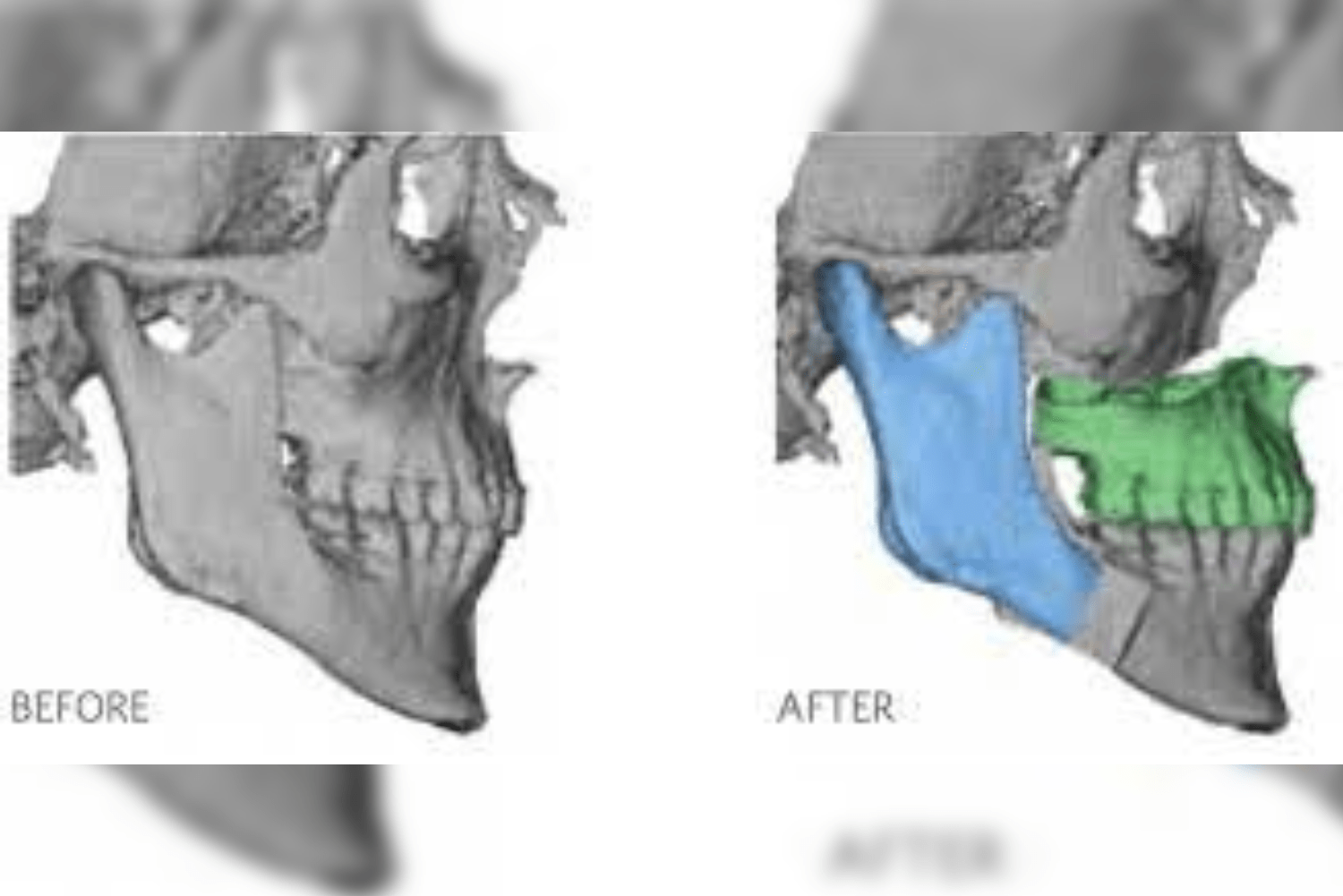
While most often cleft patients are diagnosed after birth, prenatal diagnosis of major Tessier clefts during pregnancy can be made using high-resolution ultrasound and fetal MRI. After birth, the diagnosis is confirmed and elaborated using CT scan with 3-D reconstruction to assess any bony deformity, MRI to check for brain or soft tissue involvement, and ophthalmological evaluation to assess vision-related problems. Genetic testing is also done to diagnose any syndromic involvement in the child, such as Goldenhar syndrome or frontonasal dysplasia. A multidisciplinary evaluation is essential and involves neurosurgery, plastic surgery, ENT, ophthalmology, oral and maxillofacial surgery, orthodontics, and speech therapy, along with psychological evaluation of parents and the child.
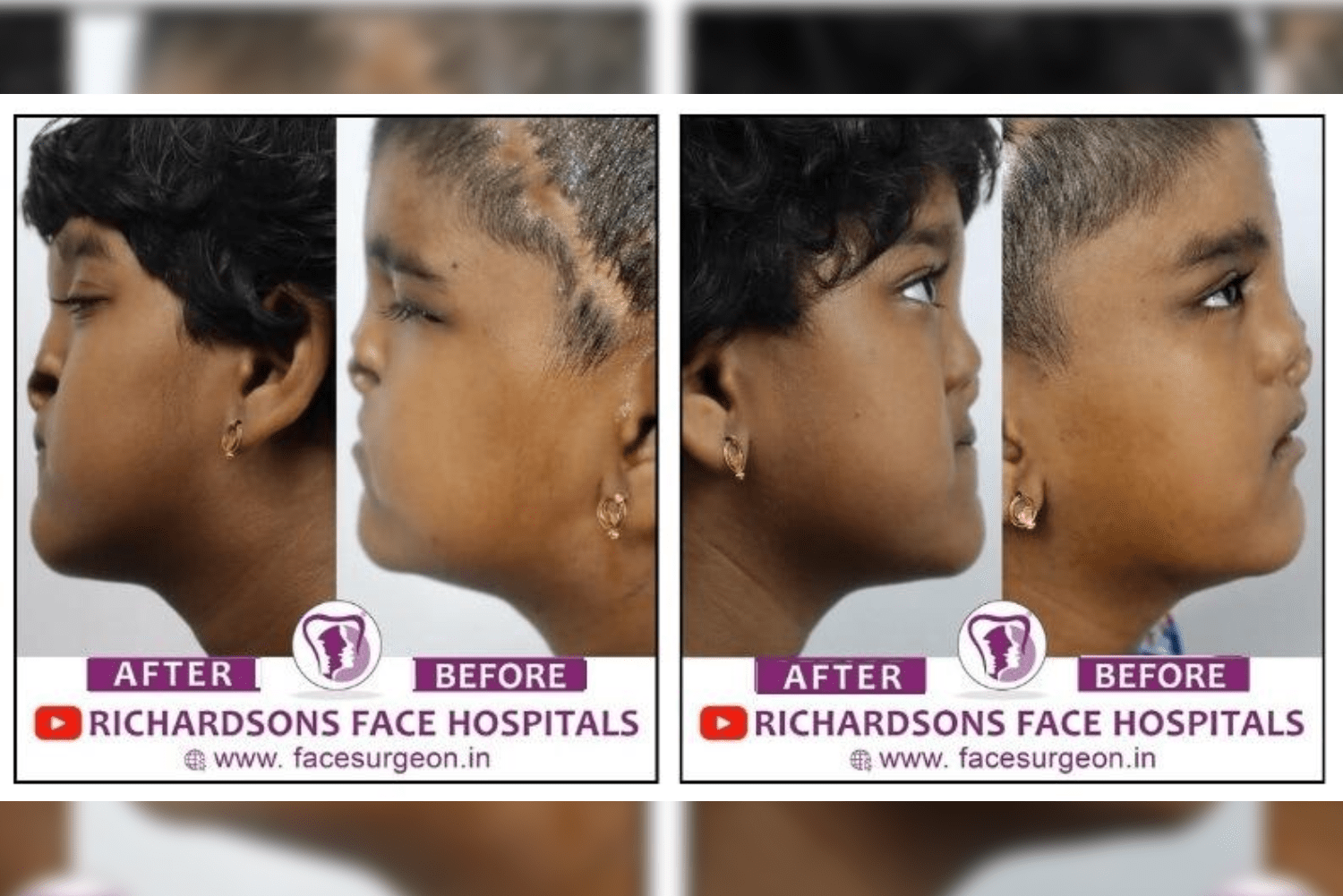
Treatment and Surgical Reconstruction
The treatment of Tessier clefts is approached in a stage-wise manner and is highly individualized, depending on the severity and extent of the cleft. The primary goals of treatment include restoring the form and function of the face, reconstructing the anatomy, and minimizing the psychosocial impact. With the complexity of Tessier clefts, long-term multidisciplinary care ensures the best possible outcomes for patients.

Timing of surgery.
Early intervention done as early as 6 to 12 months will address the life-threatening issues or the severe deformities that affects feeding or vision and also the speech. In the mid child note that is 3 to 6 years often involves major correction of bone and soft tissue along with reconstruction Since that is in the teenage involves final revisions dental restoration and cosmetic refinement that are required to phase the world with confidence with less psychosocial impact of the patient.
Surgical techniques.
Soft tissue repair involves flap reconstruction is that Plastic is local muscle reattachment to repair the soft tissue clips Reconstruction involves bone grafting distraction osteogenesis and automatic surgery to create a skeletal framework of the face. Orbital repositioning with orbital surgery is done especially in
case cases with hypertelorism and high maxillary hyperplasia. Orthognathic surgery is carried out to correct discrepancies later in adolescence to give a defined facial features to the patient Nasal and reconstruction is performed to restore both functional and appearance of the face.

The surgical complexity of the case increases with the number and severity of the cleft present, particularly when there is cranial involvement that requires neurosurgical interventions to decrease the pressure in the intracranial cavity or in the brain.
Challenges in the management.
The anatomical complexity that involves interesting clefts of multiple in numbers are an ideal example to explain why it is so difficult to correct Tessier clefts. No two clefts are identical and requires varied methods of planning to make them anatomically normal. Functional compromise is faced when there is especially issue with the airway vision and feeding. These patients require multiple surgeries and often a lifelong reconstructive journey. Due to the deformed face, speech delay and peer interaction that are addressed in stage wise these patients tend to undergo a lot of psychosocial impact which has to be supported by the multidisciplinary team approach and parents. Cost and access -a craniofacial team with specialised centre to treat such type of patients are limited globally.

Recent advancements and innovations
The field of renovation surgery has seen tremendous technological advancement that are paving road to improve outcomes in cleft management. Virtual surgical planning : It allows for the 3-D planning of complex reconstruction and provides easy notion of how the case appears post surgery during the planning itself. 3-D printing-it is used to create patient specific models surgical guides and Implants. Tissue engineering-they are used to regenerate parts of bones and cartilage. Genetic insights-prior identification of the syndrome prenatal or during pregnancy can help in better counselling and
prevention of the Clinical features. Robotic assistance surgery-this field is being explored for the
fine facial procedures thereby decreasing the time taken, injuries and the cost.
Living with Tessier Clefts
Children and adults with Tessier clefts face social stigma, emotional trauma, and educational challenges that go far beyond medical complexities. There are various support groups, counselling, and multidisciplinary teams playing a critical role in providing comprehensive care in this area.
Globally, humongous amounts of training and awareness campaigns are carried out along with specialised craniofacial foundations that work to provide free or affordable surgeries for such patients. Even though Tessier clefts represent one of the most challenging areas in craniofacial surgery, they not only require advanced surgical skills but also holistic long-term care.
The world is moving towards providing advanced medical care, better outcomes, and a chance for these children to live fuller and healthier lives. The long journey that patients with Tessier clefts undergo—from diagnosis to final reconstruction—is very complex and challenging. But with coordinated, compassionate care and continuous innovations, there is hope that every child born with such syndromes will receive impactful treatment.
If you or someone you know is affected by Tessier clefts, reach out to Richardson Face Hospital’s craniofacial team. Early intervention can make a significant difference.