Temporomandibular Joint (TMJ) ankylosis is a serious disorder characterized by restricted jaw movement, pain, and frequently noticeable facial asymmetry. It is caused by aberrant bone or fibrous tissue growth, which immobilizes the jaw joint. This illness can be brought on by trauma, infections, or other associated general body illnesses. It can have a serious negative effect on your ability to speak, eat, and carry out other basic tasks.
Because jaw function must be restored, abnormalities must be corrected, and joint fusion must not return, treating TMJ ankylosis is difficult. A combination of surgical and non-surgical methods are usually used in treatment, with the option of which to use based on the patient’s age, the underlying reason, and the degree of the ankylosis.
Restoring jaw function, reducing pain, and preventing recurrence are the goals of treating Temporomandibular Joint (TMJ) ankylosis.
In order to release the fused joint, surgery is frequently required. Treatment options include distraction osteogenesis, interpositional arthroplasty, gap arthroplasty and total joint replacement. In order to ensure long-term success and prevent re-ankylosis, postoperative care—which includes physical therapy and routine follow-up—is essential. To get the greatest results, a multidisciplinary team of surgeons, physical therapists, orthodontists, and other medical professionals is required.
Treatment with Surgery
In cases of moderate to severe TMJ ankylosis, surgery is frequently the first line of treatment. Restoring jaw movement, releasing the ankylosis, and correcting any related abnormalities are the main objectives of surgery.
Gap arthroplasty (Gap replacement surgery):
This process leaves a space between the joint surfaces by surgically removing the
fused bone. This keeps ankylosis from recurring and promotes better flexibility of
the jaw. The primary goal of gap arthroplasty is to restore movement in the
affected joint by surgically removing the ankylosed (fused) bone or tissue and
creating a gap between the joint surfaces.This gap prevents the bones from fusing
again, allowing for the free movement of the jaw.
Potential Complications:
Recurrent Ankylosis: Despite the creation of a gap, there is still a risk that the joint may re-fuse over time, particularly if postoperative care is not followed strictly.
Facial Nerve Injury: Due to the proximity of the facial nerve, there is a risk of temporary or permanent nerve damage, which can lead to facial asymmetry or weakness.
Limited Jaw Function: In some cases, the jaw may not regain full function, especially if the ankylosis was severe or longstanding.
Interpositional arthroplasty :
Interpositional arthroplasty is a surgical procedure done to treat
Temporomandibular Joint (TMJ) ankylosis, particularly in cases where
simple removal of the ankylosed tissue might not be sufficient to prevent re-fusion
of the joint. To stop re-fusion and preserve joint mobility, a graft—such as
cartilage, fascia, or synthetic material—is inserted between the joint surfaces after
the ankylosed tissue has been removed. This technique involves not only
removing the fused bone or fibrous tissue but also placing an interpositional
material between the joint surfaces to maintain the gap and allow for better long-
term jaw function. Various materials can be used for the interposition, including:
Autologous tissues: Such as temporalis muscle or fascia, costochondral graft (rib
cartilage), or dermal fat.
Alloplastic materials: Synthetic materials like silicone, Teflon, or acrylic can also
be used.
Homografts: Cadaveric grafts, although less commonly used.
Advantages of Interpositional Arthroplasty:
Reduced Risk of Re-Ankylosis: The use of interpositional material significantly reduces the likelihood of the joint surfaces re-fusing, which is a common concern after ankylosis surgery.
Improved Jaw Function: By maintaining a physical separation between the joint surfaces, interpositional arthroplasty can result in better and more sustained jaw movement compared to gap arthroplasty alone.
Customizable Approach: The choice of interpositional material can be tailored to the patient’s specific needs and the surgeon’s preference, allowing for flexibility in addressing different cases of TMJ ankylosis.
Joint reconstruction:
A costochondral graft, or rib graft, or an artificial joint prosthesis may be used to
repair the joint in situations where a considerable amount of bone has been
removed. In order to maintain healthy jaw function and restore the mandible’s
height, this is frequently done.
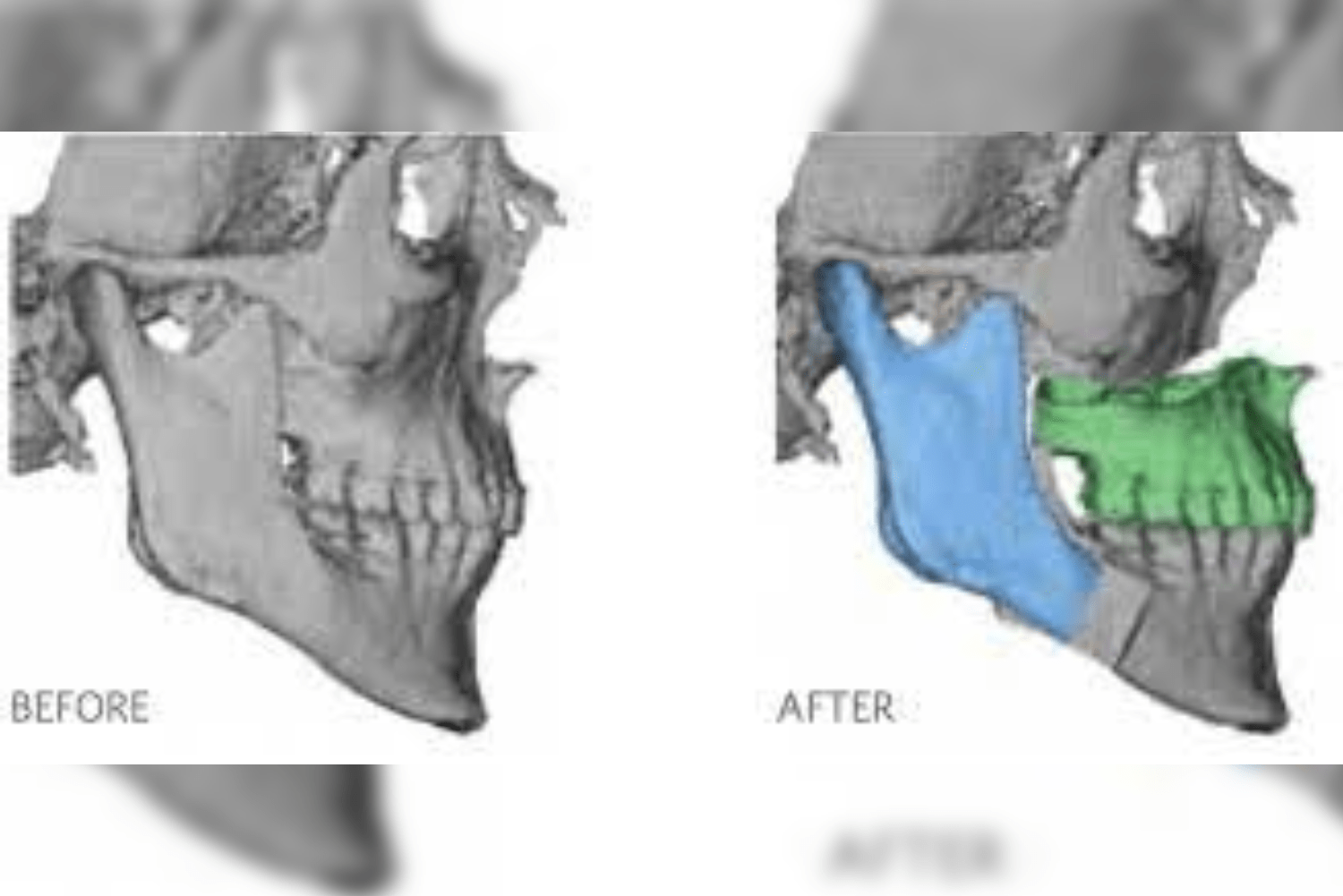
Distraction osteogenesis : Using a specialized tool, the jawbone is gradually lengthened in this method. It is a surgical technique used to lengthen bones and correct deformities, and it has been increasingly applied in the management of Temporomandibular Joint (TMJ) ankylosis. This procedure is particularly useful in cases where TMJ ankylosis has led to significant facial asymmetry or mandibular hypoplasia (underdevelopment of the jaw), especially in pediatric patients or individuals with severe deformities.
Advantages of Distraction Osteogenesis:
Gradual Correction: The slow, controlled nature of bone lengthening allows for better adaptation of the surrounding soft tissues, including muscles, nerves, and blood vessels.
Avoidance of Grafts: Unlike some reconstructive surgeries, distraction osteogenesis does not require bone grafts, reducing the need for additional surgical sites and potential complications.
Customization: The length and direction of bone growth can be precisely controlled, allowing for tailored correction based on the patient’s specific needs.
Replacement of the Total Joint (TJR): A prosthetic joint may be used to replace the TMJ in instances that are severe or persistent. This choice is usually taken into account in cases where the joint is badly injured or when all other surgical options have failed.
Non-surgical treatment options
In less severe situations, non-surgical treatments are frequently utilized to manage symptoms and enhance function in addition to surgery.
Physical therapy: Physical therapy is essential following surgery to enhance jaw movement and avoid re-ankylosis. Stretching, passive range-of-motion exercises, and jaw muscle strengthening activities are some examples of exercises.
Medication: Analgesics, muscle relaxants, and anti-inflammatory medications can all help control pain and inflammation. Injections of corticosteroids may be used to treat inflammation in some situations.
Methods for Mobilizing the Jaw: Using tools like dynamic splints or jaw stretchers as well as manual manipulation can assist preserve or enhance jaw movement during recovering.
Orthodontic treatment: Malocclusion, or misalignment of the teeth, may be caused by TMJ ankylosis or its treatment, in which case orthodontic appliances may be required.
Post-Treatment Care
Post-treatment care following the release of Temporomandibular Joint (TMJ) ankylosis is critical to ensure successful recovery, maintain jaw function, and prevent the recurrence of joint fusion. This phase involves a combination of physical therapy, medical management, dietary adjustments, and regular monitoring to support healing and long-term outcomes.
Physical Therapy:
Early Mobilization: Physical therapy should begin as soon as possible after surgery, often within the first few days, to encourage jaw movement and prevent re-ankylosis. Exercises typically include passive range of motion exercises, stretching, and gradually increasing the opening of the mouth.
Consistency: Regular and consistent therapy sessions are crucial. Patients may need to perform exercises multiple times a day, with the intensity and duration gradually increasing over time.
Use of Devices:
Jaw stretchers, dynamic splints, or other therapeutic devices may be used to assist in maintaining or improving the range of motion. These devices help in keeping the joint surfaces apart during the healing phase.
Medication Management:
Pain Relief: Pain management is important in the initial recovery phase. Patients may be prescribed analgesics (pain relievers) to manage discomfort, allowing them to participate more fully in physical therapy.
Anti-Inflammatory Medications: Non-steroidal anti-inflammatory drugs (NSAIDs) or corticosteroids may be prescribed to reduce inflammation and swelling around the surgical site, which can help in the healing process and reduce the risk of complications.
Antibiotics: If indicated, antibiotics may be prescribed to prevent or treat any postoperative infections, especially if there were concerns about infection during surgery.
Dietary Modifications:
Soft Diet: A soft or liquid diet is recommended initially to minimize stress on the jaw joint. Foods that require minimal chewing, such as smoothies, soups, and mashed foods, are ideal.
Gradual Progression: As healing progresses, patients can gradually reintroduce firmer foods, depending on their comfort level and the recommendations of their healthcare provider.
Oral Hygiene
Maintaining Cleanliness: Good oral hygiene is essential to prevent infections, particularly if there are sutures or external devices used during the healing process. Patients should follow a gentle but thorough oral care routine, as advised by their healthcare provider.
Care Around Surgical Sites: Special care should be taken around the surgical site to avoid disrupting healing tissues. The use of antiseptic mouthwash may be recommended.
Regular Follow-Up Appointments:
Monitoring Recovery: Regular follow-up appointments are crucial for monitoring the healing process, assessing jaw function, and ensuring that there is no recurrence of ankylosis. These visits often include physical examinations and imaging studies to evaluate the joint.
Adjustments and Interventions: If any complications or signs of re-ankylosis are detected, early intervention can be initiated. This may include adjustments to physical therapy, additional medications, or, in some cases, further surgical intervention.
Lifestyle Adjustments:
Avoiding Trauma: Patients are advised to avoid activities that could place excessive strain or trauma on the jaw, such as contact sports or clenching/grinding of the teeth.
Stress Management: Stress can contribute to jaw tension, which might negatively impact recovery. Stress-reduction techniques, such as relaxation exercises or counseling, can be beneficial.
Long-Term Considerations:
Orthodontic Treatment: In cases where malocclusion or misalignment of the teeth has occurred due to TMJ ankylosis, orthodontic treatment may be necessary as part of the long-term care plan.
Speech Therapy: If jaw movement was significantly restricted prior to surgery, speech therapy might be needed to help improve speech articulation and swallowing function.
Conclusion
The management of TMJ ankylosis is a complex process that calls for a blend of non-surgical and surgical methods in order to relieve pain, restore jaw function, and stop the condition from returning. Particularly in extreme situations, surgery is frequently the mainstay of care. Total joint replacement, joint reconstruction, and arthroplasty are prominent surgical techniques. For long-term care and post-surgical healing, non-surgical techniques including physical therapy and medicines are essential.
Early diagnosis, meticulous surgical planning, and conscientious postoperative care are essential for successful therapy. To get the greatest results, a multidisciplinary team of physical therapists, surgeons, and other experts is required. Many patients can regain significant jaw function, enhance their quality of life, and lower their risk of developing difficulties in the future with prompt and proper care.