Obstructive sleep apnea (OSA) is a problem in which breathing stops for a brief period during sleep that occurs due to narrowing or blocking of the airway. Many factors, like jaw deficiencies, large tongues, tonsils, and adenoids, may obstruct the flow of air through the airways, causing oxygen deficiencies, due to which a person wakes up momentarily to resume normal breathing. This results in daytime sleepiness, drowsiness, memory loss, headaches, and withdrawal from social life. In the extreme case, it can cause stroke and even death.
A polysomnograph (PSG) also known as sleep study is a gold standard for diagnosing OSA. Currently, a continuous positive airway pressure (CPAP) device is considered the first line of treatment for OSA. However, most of the patients are not tolerant of CPAP. In such cases, alternative treatment options are considered and the surgical approach is one among them. The goal of surgical therapy for OSA is to enhance airway patency by treating the specific blockage site. The blockage/constriction can occur in any location within the airway; hence, different surgical procedures are developed accordingly.
INDICATIONS OF SURGERY:
Surgery is a primary treatment option for those with noticeable physical abnormalities such as enlarged tongue, tonsils, adenoid, jaw deficits, collapsed palate, and nasal issues. It is also a treatment option for those who are not compliant with CPAP therapy. One more indication is when patients reject all other treatment options and insist on surgery.
PRESURGICAL EVALUATION:
The location of the blockage cannot be determined by PSG, despite it being the gold standard for diagnosing OSA. Physical examination of the nose, throat, tongue, and nasopharyngoscopy (a fiber optic wire with a camera and light is inserted through the nose to the throat, and an obstructed area is visualized) and sleep endoscopy (similar to nasopharyngoscopy but done under mild sedation) are required to assess the upper airway and locate the area of obstruction.
In addition, imaging such as a lateral cephalogram, 3-dimensional cone beam computed tomographic scan, and magnetic resonance imaging (MRI) is also done to capture real-time images and know at what level obstruction is present. Based on PSD data, physical examinations, and images, the area of blockage is identified, and proper surgical treatment is planned.
Before the surgery, patient counseling is done, where discussion regarding the area of obstruction, the procedure of the surgical procedure, benefits and complications are explained, and consent is taken.
TYPES OF SURGERY:
The blockage site(s) determines the surgical treatment plan. Surgery may involve skeletal alterations or the removal of soft tissues. Surgeries are performed on the nose, tongue, palate, bones of the face, neck, and jaws, and soft tissue at the back of the throat.
- Nasal surgery: Whatever is obstructing your nasal canal is eliminated or reduced in size. This includes turbinates (curved bones that run down the side wall of your nose) and soft tissue growths known as polyps. The deviated/crooked septum (bony structure that divides the nose), which can cause difficulty in breathing, is straightened.
- Surgeries of the tongue: Excess tissue at the back of the tongue may reduce free air movement. Tongue reduction is the procedure where the tongue base’s overall size is reduced. Sometimes tongue muscle is pulled forward and attached to the chin so that it should not block the airway.
- Surgeries to palate and throat: The soft tissue of the palate (roof of the mouth) and side of the throat is reshaped by the surgeon by various surgeries.
- Uvulopalatopharyngoplasty (UPPP) is where the surgeon removes all or some part of the uvula (the soft tissue that hangs down at the back of the throat), parts of the palate and tissues on the side of the throat along with tonsils (two lymph nodes at the back of the throat) and adenoids (tissue at the nose). Patients recover within 2–3 weeks. A few complications like voice change and swallowing difficulty can be noticed.
- Uvulopalatoplasty: laser beam (strong light that cuts tissue) or cautery (heat from electric current is used to cut tissue) may be used to resect the uvula and palate tissues. It is an in-office procedure and does not require the patient to be admitted to the hospital. A sore throat may be present after surgery.
- Palatal implants: The doctor numbs the throat and places mini plastic rods, surgically in the soft palate to stiffen the tissue and modify the air flow in the throat.
- Tonsillectomy and adenoidectomy, i.e., removal of tonsils and adenoids, are done if they are swollen and hinder air passage; usually children with sleep apnea need this surgery.
- Surgeries of jaws:
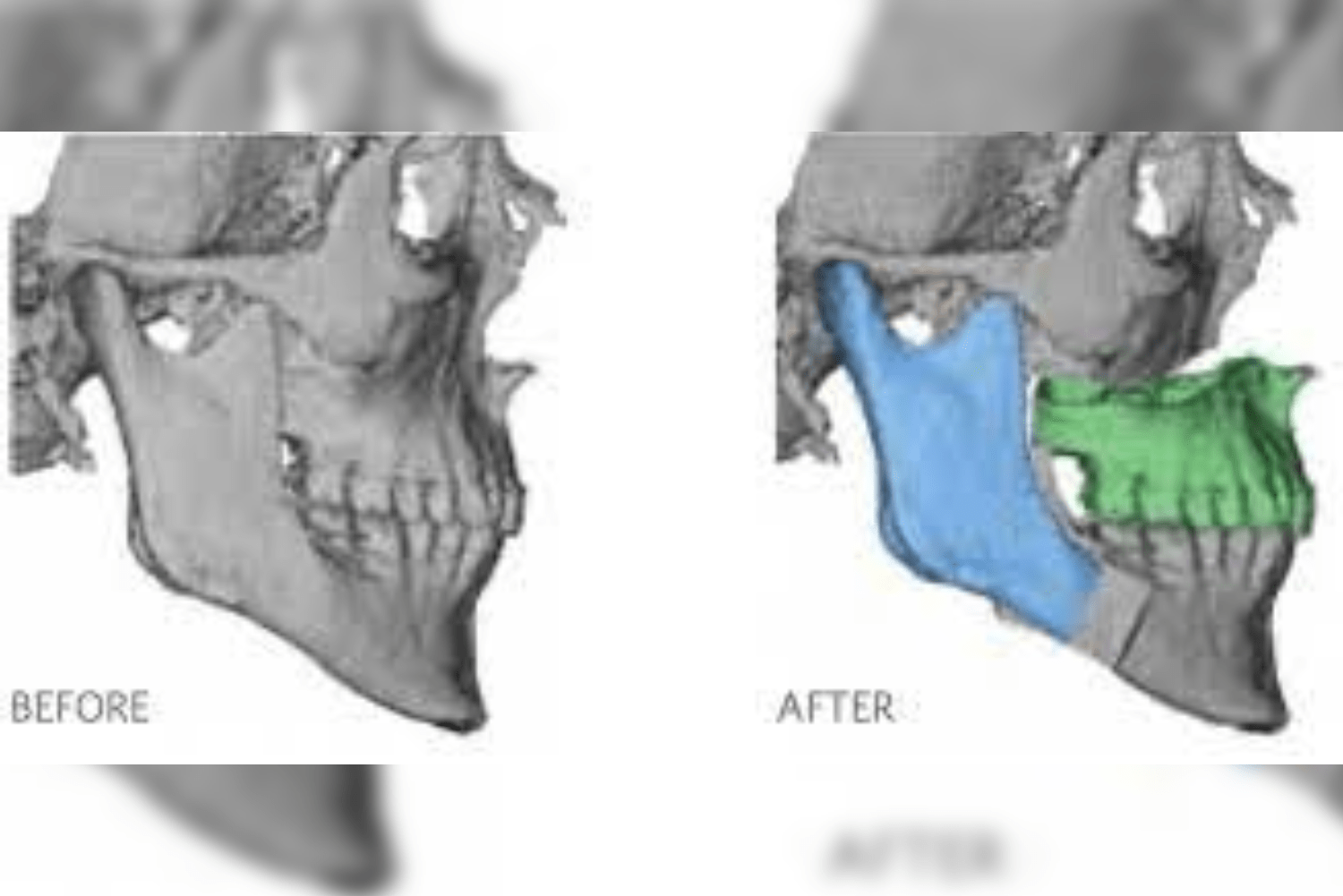
- Maxillomandibular advancement (MMA): This technique widens the upper airway by moving the upper and lower jaws forward by around 10 millimeters. The soft tissues that are linked to the face bones are likewise pulled forward by its advancement; this creates space in the back of the throat. Due to various complications and side effects, this is not preferred and reserved as the last phase of surgery.
- Genioglossus advancement: The tongue is held in place by lower jaw. Your tongue will be pushed back too far if your lower jaw is too narrow and which will restrict the amount of air in your throat. It is referred to as tongue base collapse. A minimally invasive surgery is performed where involves the surgeon separates and moves the chin bone forward. The tongue will get firmer as lower jaw is drawn forward, decreasing the likelihood of obstruction of the airway as a person sleeps.
- Maxillary expansion (distraction osteogenesis): whenever there is a smaller upper jaw, nasal space also becomes constricted. In such cases, a custom-made expander is made by the dentist and inserted into the mouth over the palate with the help of mini implants. The surgeon makes an incision in the center of the roof of the palate to create a tiny gap. After a week, the patient will use the key to move the two halves of the expander away from each other every day. This creates the gap and opens up the upper airway.
- Tracheostomy: The physician will create a tiny incision in your windpipe. At night, you would breathe through a special tube. This implies that you wouldn’t even need to use your upper respiratory tract. During the day, the hole can be covered. In this manner, you may inhale and speak normally. This is a last-resort treatment that could help your OSA.
- Bariatric Surgery: surgery done to help obese people lose weight. Here changes are made in the digestive system. It is done by altering the size of the stomach, altering the nutrient absorption, and altering hormone levels responsible for hunger.
- Hypoglossal nerve stimulation (HNS): it is not a surgery. Here, a pacemaker-like device is inserted into the chest, and a wire is attached to the hypoglossal nerve (the nerve responsible for tongue movement). When a person sleeps, electric signals trigger the nerve, pushing the tongue in a forward direction.
CONCLUSION:
Patients should be offered CPAP therapy before surgery. Other conservative approaches like weight reduction, physical exercise, positional therapy, and oral devices should be considered before moving ahead with surgery. When these options fail, as a last resort, surgery should be considered. Surgical therapy significantly enhances patients’ quality of life and survival, especially anatomical abnormalities causing OSA can be corrected. OSA is a chronic disease that requires long-term follow-up. Constant monitoring is required to prevent recurrences and worsening of OSA.