Post-Cancer Facial Reconstruction:
After battling oral cancer, the patients are faced with the challenging reality of physical deformities that result from treatment.
● These changes can vary a lot depending on the type of cancer and treatment, but the impact of the major surgery and the adjuvant therapy can be devastating in the aesthetic and the functional sense. Post-Cancer Facial Reconstruction aims to address these changes and restore facial appearance.
● Whether it’s a change in the appearance of the face or difficulty in speaking/eating and swallowing, these physical changes can deeply affect not only one’s health but also one’s emotional well-being. Post-Cancer Facial Reconstruction helps improve both function and confidence.
● Psychosocial, vocational and emotional counseling are more often than not necessary for total recovery.
● Examples of aesthetic consideration include improving the contours and expressions of the face.
● Functional concerns warrant consideration that include speech, chewing and swallowing.
● Restoration of oral competence is necessary in an effort to achieve total rehabilitation.
● The main purpose of correction of post-cancer deformities is allowing patients to regain their confidence and improve their quality of life through the restoration of function and appearance.
Here are some common changes that may occur post cancer surgery:
a. Surgical scars:
➔ After surgery of the head and neck, scars around the face, jaws, neck are inevitable. The extent and visibility of scars depend on the type and location of the surgery. Post-Cancer Facial Reconstruction can help minimize the appearance of these scars.
➔ In surgeries where large portions of the skin that is affected by cancer are removed, skin grafts from other parts of the body are used and these can leave noticeable scars or even create changes in the skin texture.
b. Facial asymmetry:
➔ Surgical resection of tumour and adjuvant chemoradiotherapy often results in facial disfigurement due to the removal of large parts of tissues from the jaws, tongue, palate or muscles of the mouth. Post-Cancer Facial Reconstruction aims to restore symmetry and improve facial aesthetics.

Changes in Skin:
➔ Hyper/Hypo pigmentation: Radiation and chemotherapy, although beneficial in eliminating remaining cells of cancer, tend to come with their own set of adverse effects. The irradiated area tends to show changes in skin pigmentation, causing these areas to become darker (hyperpigmentation) or lighter (hypopigmentation) compared to the surrounding normal tissues. Post-Cancer Facial Reconstruction can help in restoring a more even skin tone.
➔ Tightening of Skin: Irradiated skin is usually tight or stiff, particularly around the cheeks, neck, and throat.
➔ Sensitivity and changes in appearance: Post chemotherapy and radiotherapy, skin tends to be more sensitive to sun exposure, changes in temperature, or even to the application of certain skin products that can cause dryness, redness, and thinning of the skin. Over time, these changes can lead to wrinkling or even a leathery appearance of the skin, which might be permanent. Proper Post-Cancer Facial Reconstruction can address these skin changes and improve overall facial aesthetics.
c. Hair loss/Alopecia:
➔ Hair loss on the scalp is a common side effect of chemotherapy and it is usually temporary until the patient is on chemotherapy treatment. In some cases, hair grows back with a different texture, color, and is sometimes very scanty. Post-Cancer Facial Reconstruction may include options to restore facial hair, eyebrows, and eyelashes to improve appearance and confidence.
➔ Eyebrow and Eyelash Changes: Eyebrows or eyelashes usually take longer to grow back, or might not return fully.
d. Facial fat redistribution:
➔ Surgery and chemoradiotherapy may cause changes in facial fat distribution. Post-Cancer Facial Reconstruction can address these changes to restore natural facial contours.
➔ Most treatments cause fat loss in the face that leads to a more hollow/gauntish appearance, especially in the cheeks or under the eyes.
➔ On the other hand, some people may develop a “moon face,” i.e., a round or puffy face due to the long-term use of steroids.
e. Changes in mouth:
➔ Surgery may cause deviations in the jaw that may cause reduced mouth opening, which can be addressed through Post-Cancer Facial Reconstruction.
➔ Radiation, especially when it’s targeted at the head or neck area, can impact dental health and hence cause difficulty in chewing.
➔ The most common side effect of radiotherapy is dry mouth, also known as xerostomia, and tooth decay.
g. Psychological and Emotional Impact:
➔ Each person’s experience with facial changes post-cancer is unique, and some of the effects may improve over time through Post-Cancer Facial Reconstruction.
➔ However, changes in appearance can affect self-esteem and emotional well-being.
➔ Some people even experience feelings of anxiety and depression related to how they perceive their facial appearance.
● DEFORMITY CORRECTION:
a. Surgical Reconstruction:
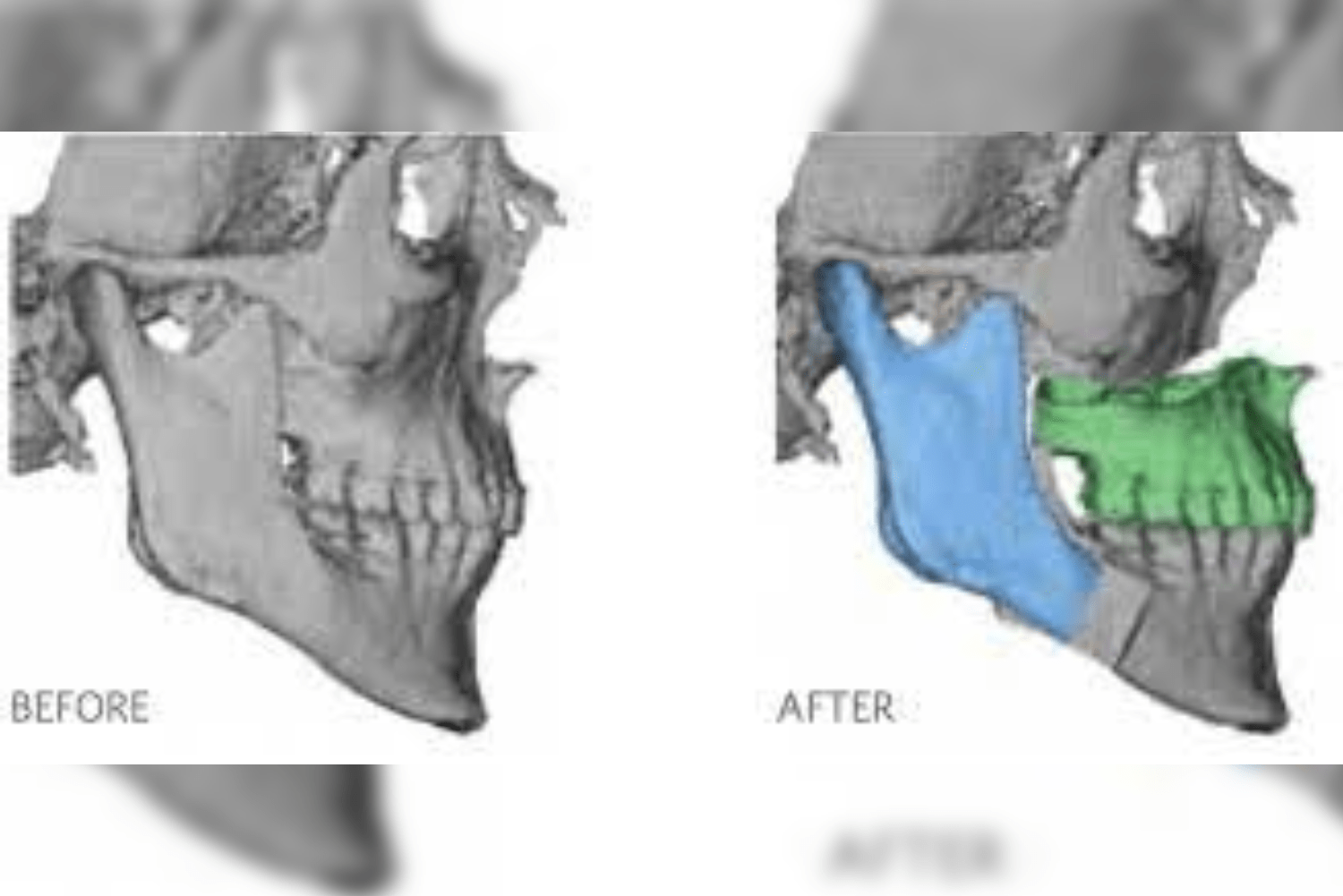
➔ Patients who have had a part of the jaw, tongue, or any part of the mouth removed, reconstructive surgery is planned to rebuild that part of the jaw, tongue, or mouth. This is part of Post-Cancer Facial Reconstruction.
➔ Soft tissue and bone reconstruction often involves grafting tissue, i.e., either muscle, skin, or bone from other parts of the face (local tissue transfer) to rebuild the affected area.
➔ Microvascular surgery—In cases where tissues are taken from a distant site such as the thigh, forearm, leg, shoulder, back, or chest and reattached with its own blood vessels to the operated site, it is called free flap tissue and is an advanced form of Post-Cancer Facial Reconstruction.
➔ Microvascular surgery is much more complex and involves an experienced team of doctors specialized in this type of surgery.
➔ Reconstructive surgery can be performed as part of the resective surgery, where, along with the surgical removal of the primary tumour, its reconstruction is also planned.
➔ Two teams of doctors are involved in the same surgery, one for the surgical removal of the tumour and the other for the harvest of the flap and reconstruction.
➔ Reconstructive surgery can also be planned as a separate second surgery after the removal of the primary tumour, completing the process of Post-Cancer Facial Reconstruction.
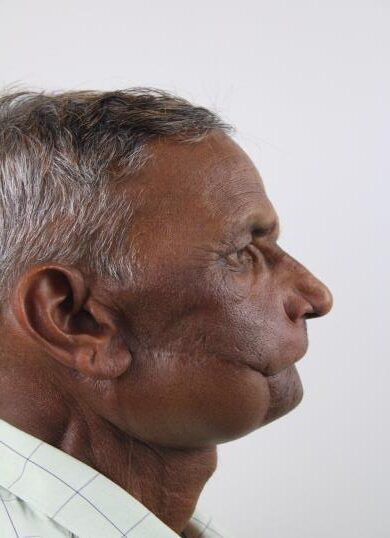
Facial Deformity Post Cancer:
Face Reconstruction with Custom-Made Patient-Specific Implants:
Mouth Opening Achieved with Nasolabial Flap Reconstruction:
Bilateral Nasolabial Flap Reconstruction with Coronoidectomy for Mouth Opening:
Temporal Hollowness and Maxillary Deficiency Corrected with Bilateral Nasolabial Flap Reconstruction:
Flap Debulking and Jaw Sculpting Surgery Post Cancer:
Jaw Reconstruction with Leg Bone (Fibula Flap):
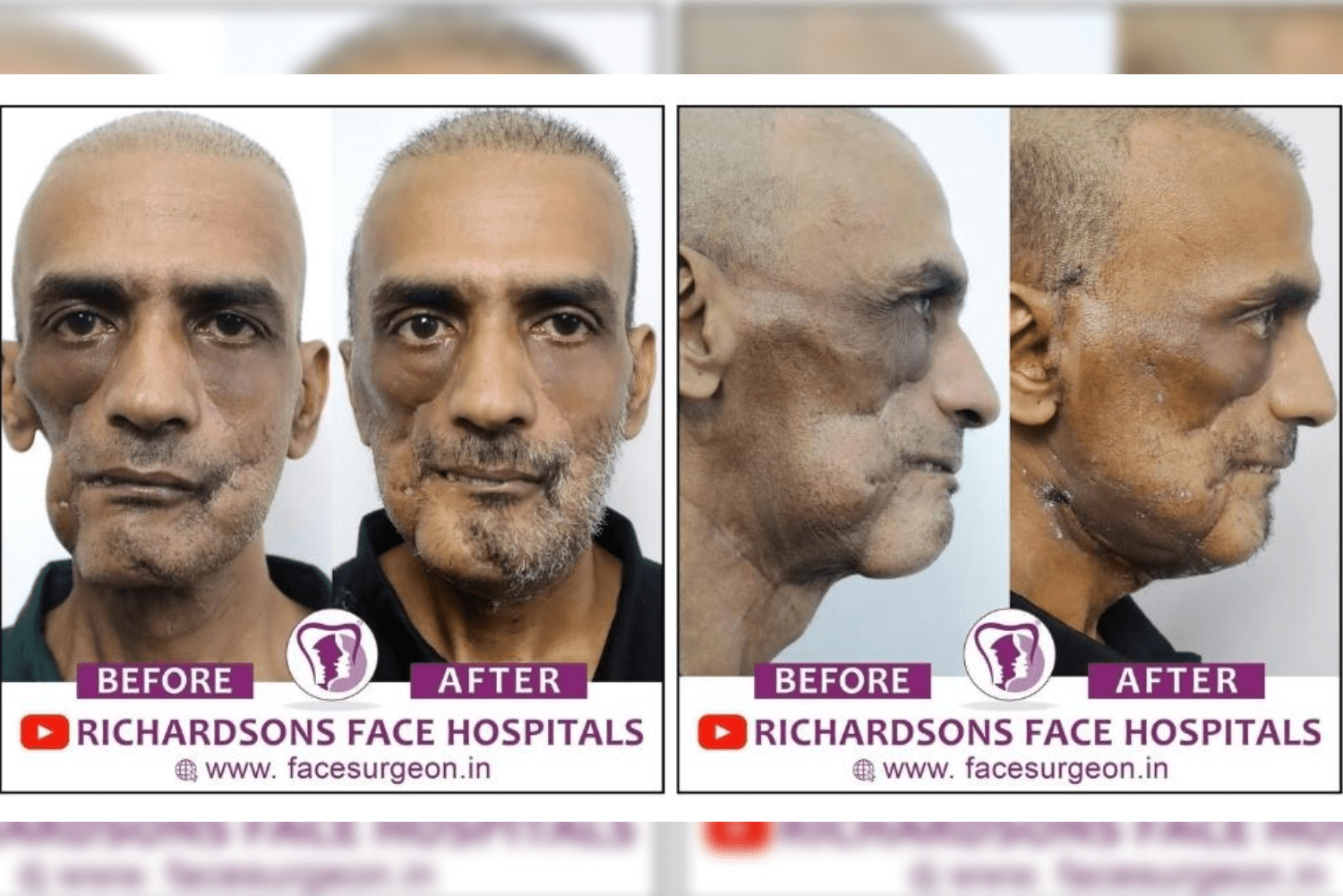
Face Makeover Surgery Post Cancer Surgery:
Improving Mouth Opening with Nasolabial Flap:
b. Maxillofacial Prosthetic Rehabilitation:
➔ In case of a surgical defect that cannot be reconstructed with any autogenous flaps/grafts, then the defect is filled with a prosthesis.
➔ The fabrication and fixation of such prostheses for people who have lost parts of their face or skull, is termed as maxillofacial prosthetics.
➔ Specialist dentists known as Prosthodontists are responsible for the creation of maxillofacial prosthetics customised to the patient.
➔ These prostheses are customised to exactly contour the individual’s defect, thus causing a functional improvement along with the aesthetic restoration of the face. In many cases, this is an integral part of Post-Cancer Facial Reconstruction to restore both appearance and functionality.
➔ Prosthetic noses, palates and eyes are used to restore the natural shape and function of the face. These devices help patients feel more like themselves and comfortable in social situations.
➔ Obturators are removable prosthetic devices used to close the opening in the mouth after the surgical removal of a part of the palate or jaw. They restore the ability to eat and speak along with the improvement in the appearance of the face. Such prosthetic rehabilitation plays a vital role in Post-Cancer Facial Reconstruction, ensuring patients regain confidence and better quality of life.
➔ Maxillofacial prosthetic placement post resection of jaw
Watch video

c. Dental Rehabilitation:
➔ In most surgeries, teeth or even parts of the gums are removed to remove the cancerous lesion in its entirety.
➔ Thus, rehabilitation with dentures, crowns, or dental implants becomes necessary to restore the ability to chew and smile.
➔ This is important not only for eating but also for improving the patient’s self-esteem. Dental rehabilitation is often considered an essential step in Post-Cancer Facial Reconstruction, as it restores both function and aesthetics.
➔ Achieving mouth opening post cancer surgery –
Watch video

d. Scar Management:
-
Scar Revision Surgery: Scar revision procedures can be performed to reduce the surgical scar.
🔗 Scar revision surgery post cancer -
Scar Lightening Treatments:
-
Topical application of creams containing tretinoin, hydroquinone, or vitamin C.
-
The application of silicone gel sheets can significantly fade surgical scars.
-
Chemical peels, laser treatments, dermabrasion, or microneedling may also help lighten scars and improve texture, making them less noticeable over time.
-
-
Non-surgical aesthetic procedures: Botox, dermal fillers, PRP therapy, steroid injections, cryotherapy, etc., can be used to correct minor facial asymmetries.
-
Fat Grafting: Deficient areas of the face can be treated by harvesting fat from the patient’s abdomen or thigh.
-
Hair Transplantation: Hair transplantation on the scalp, eyebrows, moustache, or eyelash region can be attempted for patients experiencing hair loss after treatment.
-
Our Dermatology/Cosmetology department has doctors who are well-trained in these procedures.
🔗 Face makeover surgery post cancer
e. Speech and Swallowing Rehabilitation:
-
Speech and Swallowing Therapy: Therapists work with patients to regain their ability to speak clearly and swallow easily after the removal of parts of the tongue, palate, or throat.
-
Muscle Retraining: Specific exercises are taught to retrain the muscles involved in speech and swallowing, helping reduce the risk of choking and aspiration.
f. Physiotherapy:
-
Strength and Flexibility: Physiotherapy helps restore the strength, flexibility, and mobility of the jaw and neck muscles affected by cancer surgery.
-
Functional Improvement: Exercises focusing on jaw movements, neck strength, and posture aid in improving normal speech and eating functions.
g. Long-Term Follow-Up Appointments:
➔ Regular follow-up consultations are essential, usually with CT/MRI/PET scans, to monitor the disease and to catch any spread to other regions, potential complications, or even for the adjustment of prosthetic appliances as and when required.
➔ Yearly visits post cancer surgery with the oncology team and other specialists ensure that patients continue to heal physically and emotionally. Consistent monitoring is a crucial part of Post-Cancer Facial Reconstruction, helping patients maintain both functional recovery and long-term quality of life.












3 Responses
Very good
Good
Awesome