Obstructive sleep apnea occurs when the airway partially or completely collapses repeatedly throughout the night. This results in breathlessness, causing the person to wake up long enough to start normal breathing, subsequently causing disrupted sleep. A person experiences insomnia, excessive daytime sleepiness, drowsiness, irritation, and headaches hindering his daily activities. Initial diagnosis is made based on these symptoms, medical history (alcohol, smoking), and physical examination of the throat, mouth, and nose. However, polysomnography remains the gold standard to diagnose OSA.
POLYSOMNOGRAPHY
Polysomnography (PSG), also called sleep study, is an important part of many sleep evaluations. When it comes to identifying sleep-related breathing disorders (SRBD), such as obstructive sleep apnea (OSA), PSGs are the gold standard. This method is also quite popular and useful in the diagnosis and treatment of a wide range of sleep-related disorders. This study records information from several bodily systems, such as the heart, brain, lungs, and other vital organs, while you are asleep. Data collected from these records are studied, and a diagnosis is drawn. This test normally takes one night to complete and is not painful. It can be done at home or in hospital settings.
- WHEN IS IT NECESSARY?
Sleep study is not only used for diagnosis of OSA but also to rule out other sleep-related disorders such as
- Insomnia
- Restless leg syndrome
- Panic attacks during the night
- Sleep paralysis
- Sleep walking
- Sleep terrors
- Epiletic attacks during the night
However, it is not necessary to perform this test in common events like sleep talking, teeth grinding habits, and so on.
- WHAT TIME IS THE STUDY CONDUCTED?
It is normal to conduct the test during normal sleeping hours, i.e., nighttime; however, it can also be conducted during the daytime if a person works an overnight shift.
- WHO PERFORMS SLEEP STUDY?
The sleep study team consists of healthcare professionals such as licensed medical technicians, assistants, and nurses who perform and record the readings. They then submit this data to a sleep specialist, who reviews the records. They work together with a pulmonologist (specializing in lungs), an otolaryngeologist (ear, nose, and throat specialist), a neurologist (brain specialist), a psychiatrist (specializing in treatment of mental health conditions), and a dentist (oral health specialist) to diagnose and plan treatment. The team may involve other specialists, such as surgeons if required.
- HOW IS THE STUDY PERFORMED?
Initial assessment:
A detailed medical history (medication, alcohol, smoking, etc.) and careful physical examination are performed. Sleep histories for the last 24 hours are taken and are asked to fill out containing certain questions regarding their sleep.
Patient instruction:
- Patient should report one hour prior to scheduled time.
- A prior visit if necessary to familiarize with the study surrounding.
- Avoid daytime sleep as it can make it difficult for you to sleep during study.
- Avoid alcohol, smoking, and stimulants such as caffeine on the day of study, which can disrupt your normal sleep pattern.
- Avoid strenuous exercise and have a relaxed day on the day of PSG.
- Inform the healthcare specialist regarding the medication you take on a daily basis. Depending on that, the provider may ask you to either continue or stop the medication on the day of study.
- Inform regarding sensitive skin or skin allergies beforehand.
- Carry comforting clothes, and if possible, take a relaxed shower before starting the study.
Components of PSG:
There are numerous factors that can affect your sleep. Healthcare professionals may examine your sleep in great detail by using a variety of sensors, each of which tracks a different bodily system or function. It include
- Electroencephalography (EEG): Sensors are attached to the head to measure the electrical activity in the brain.. Different patterns of signals are produced during different phases of sleep. It is a crucial method for determining sleep problems.
- Electrocardiography (EMG): Sensors are attached to the chest to measure the record heart’s electrical activity. This tracks the rhythm of the heart and electrical changes in it.
- Electromyography (EMG): it measures the muscle movement. Usually these are attached chin and legs.
- Electro-oculography (EOG): sensors are placed above and below eyes and measure eye movements.
- Pulse oxymeter: attached to index finger of hand and measure the oxygen level of blood and heart rate.
- Position monitor/video monitor: to record change in body positions
Respiratory monitoring is done by various equipment.
- Thermocouple: placed between mouth and nose. Monitors airflow by detecting changes in temperature.
- Respiratory inductive plesthesmography: belts with sensors are placed around the torso. It records the movement of the chest and stomach.
- Snoring monitors: a small microphone is placed on the patient’s neck to record the audio.
How are the settings in the recording room?
Patients and technicians are placed in adjacent rooms. Room has a soundproof intercom system to interact with patients if necessary. It is equipped with soothing light for proper sleep. Video and audio monitoring is done by technicians to see and hear what is happening during sleep or in case any emergency is required.
How is the procedure performed?
It takes place in a specialized sleep center or hospital setting. Patient is accommodated in a room, and technologists will place sensors on chest, head, chin, around eyes, and legs with the help of adhesive tape or glue-like substance. A clip-like device is placed on the finger. These sensors are connected to computers or monitors by wires, which show the changes in the body and record them. They may ask you to perform certain movements, such as raising legs or blinking, to check if the sensors are working. The wires of sensors are long enough to allow body movement. After you fall asleep, technologists monitor the patient throughout the night or sleep. In the morning, when the patient wakes up, sensors are disconnected, and the patient is sent home.
After the study, the data is reviewed and studied by the sleep study team, and a diagnosis is made based on the data. If the disorder is confirmed, a follow-up visit is made and treatment options are discussed.
- WHAT ARE THE COMPLICATIONS?
No potential complications, but sometimes skin irritation may arise due to the attachment of sensors to the skin.
- WHAT CAN INTERFERE WITH THE STUDY?
- First-night effect: troubled sleep due to unfamiliar setting
- Changes in medication can interfere with the quality of sleep.
- TYPES OF POLYSOMNOGRAPHY
- Overnight PSG: gold standard test to diagnose OSA. Here the person spends the night at a sleep center or hospital-based center, and technologists monitor them. Brain activity, eye movement, heart rate, respiratory rate, oxygen levels, movements, and snoring are recorded.
- In-home PSG: done in person’s home. Either you can pick up the equipment from the study center or technicians will reach your location and fix the equipment and educate you on how to wear and remove it. Respiratory rate, heart rate, oxygen levels, and snoring are recorded, but not brain activity. It is not recommended for people with serious health issues such as heart diseases.
OTHER DIAGNOSTIC AIDS
- Nasopharyngoscopy: performed in a hospital facility where a flexible tube with camera and light is inserted through the nose into the throat. This helps visualize the organs that can hamper airflow.
- Sleep endoscopy: it is similar to nasopharyngoscopy but is performed by administering sedative drugs.
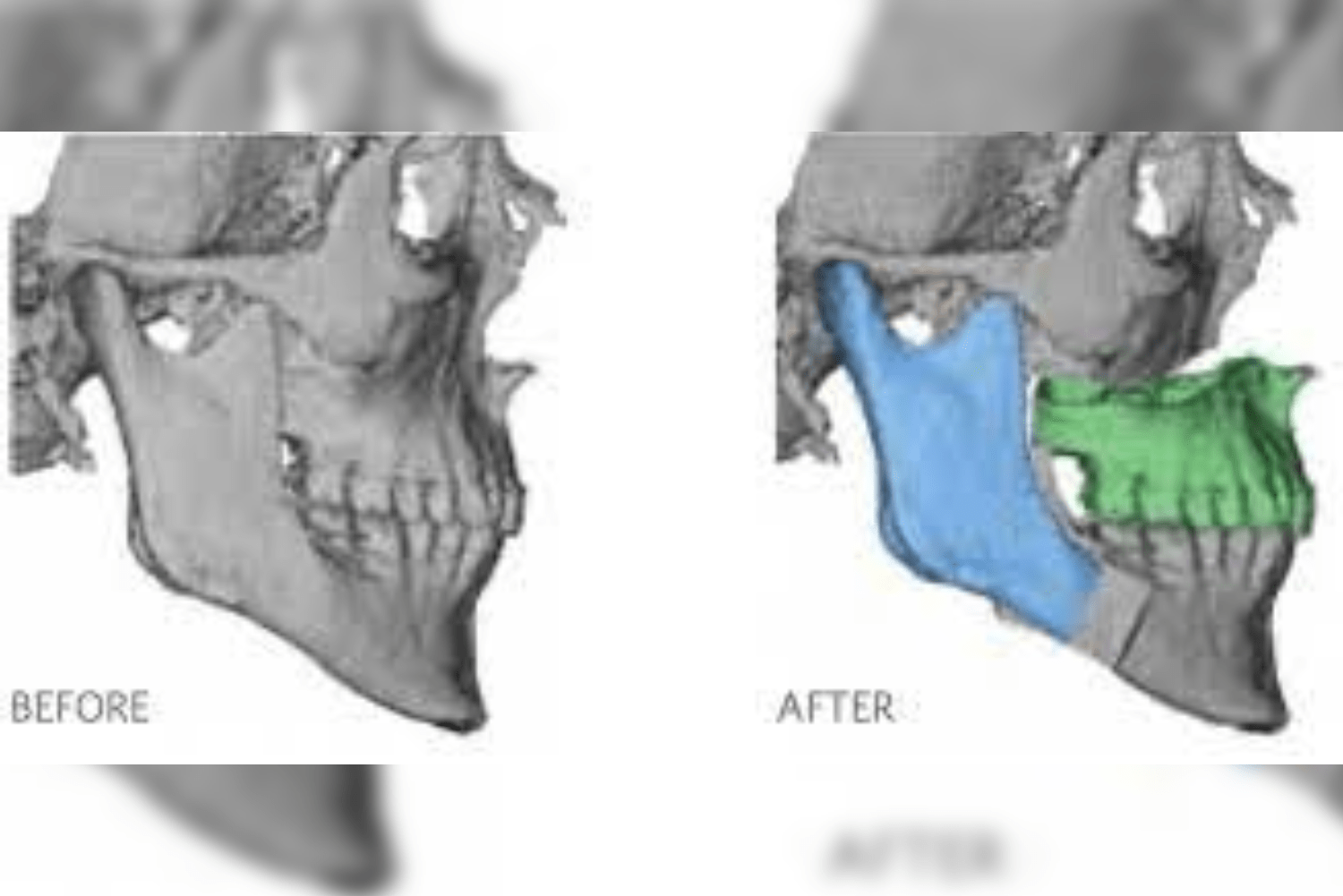
- Imaging techniques such as magnetic resonance imaging (MRI), computerized tomography scans (CT scan), cone beam computed tomography (CBCT), and lateral cephalograms can also provide possible information regarding obstructing areas in the respiratory system.
CONCLUSION
Sleep disorders can have a great impact on physical and mental health. When left undiagnosed or untreated, patients experience misery. While various diagnostic aids are available, polysomnography plays a crucial role in identifying sleep disorders. Possible attempts have to be made to diagnose OSD as early as possible.