Lower jaw fracture treatment, also termed as mandibular fracture, is the second most common fracture of facial bones, the first being the fracture of the nose. It is predominantly noted in men than in women and is highest seen in the age group of 20–30s.
When your lower jaw starts aching after a fall or assault, it is overlooked for the presence of any fracture.
It is most painful when the jaw movements are made, and further examination will specify whether it’s a broken bone or injury to your muscles and soft tissues only. Proper and timely lower jaw fracture treatment helps in restoring normal function, reducing pain, and preventing long-term complications.
Causes Of Jaw Fracture
Various causes of jaw fractures are present. They are:
- Road traffic accident: This is one of the most grievous injuries that reports with multiple bone fractures and sometimes only with mandibular fracture. A term called dashboard injury is used, as most people tend to hit their chin on the dashboard of cars during a road traffic accident. This leads to a fracture in the chin or the condyle region (near the ears where the jaw movements are felt), requiring timely lower jaw fracture treatment to restore normal function and prevent long-term complications.
- Assault / hit by another person: assault by any person leads to fracture of facial bones. The hit by fist to the chin or cheek or using any weapon can lead to the fracture of facial bones.
-
Self fall: Accidental self-fall, or a slip on the floor, leads to fracture of the bones, often sparing the head injury at times. The mandible is the first bone that comes in contact with the floor during falls, and in such cases, timely lower jaw fracture treatment is essential to restore function and avoid further complications.
-
Work-space injury : the industrial injury commonly reports soft tissue injury than fractures. But the incidence of jaw bone fractures is still high. The cutting and trimming machinery used in the industries are the most common source of injury to the face.
-
Dental procedures: Dental procedures like removal of impacted tooth have reported incidences of lower jaw bone fracture. It is because the impacted tooth generally makes the lower jaw bone weaker, and during removal, the force applied can break the cortical plates of the bone. In such cases, proper lower jaw fracture treatment ensures stability, healing, and restoration of normal jaw function.
How To Know Whether It Is A Fractured Bone?
When your jaw bone seems to be fractured you can have a small check of it yourself.
-
If any teeth are missing: It’s always better to carry the broken teeth with you, if by any chance you happen to collect them at the accident site. Immediate evaluation helps in planning proper lower jaw fracture treatment.
-
Mobility in the jaws: The lower jaw may start moving into pieces of two or rarely three. This instability requires urgent medical attention and sometimes surgical lower jaw fracture treatment.
-
Severe swelling: Swelling is the first reaction that the body shows when there is any injury. But when there is a fracture, the swelling will be higher than soft tissue injuries.
-
Bleeding from the mouth: A fractured bone with breach in the soft tissue covering will lead to bleeding from the mouth or nose.
-
Unable to swallow or breathe: When the jaw bone is fractured, there will be difficulty in swallowing food and sometimes even breathing, as the support to the jaw is impaired.
-
Inability to open the mouth: Jaw bone fracture often restricts mouth opening due to overriding of fracture segments or spasm of muscles responsible for jaw movements.
-
Deranged occlusion: This is the most common finding in a fracture. As the jaw bone shifts to a new position upon fracture, the teeth don’t come in contact with each other. Normally, there is a fine adjustment between the upper and lower teeth that make them occlude in a certain position. Any changes in this will make the teeth change their contact and lead to difficulty in chewing food, highlighting the need for immediate lower jaw fracture treatment.
Who to Contact In Case Of Fracture?
The specialty that deals with jawbone fractures is oral and maxillofacial surgery. These trained specialists provide lower jaw fracture treatment by fixing the jawbone back to its original position while taking care of occlusion to ensure optimum mouth functionality.
When you see your healthcare provider during the initial checkup, make sure you are referred to an oral and maxillofacial surgeon to receive proper lower jaw fracture treatment.
How Is It Treated?
Jaw bone fracture treatment depends on the site and type of fracture.
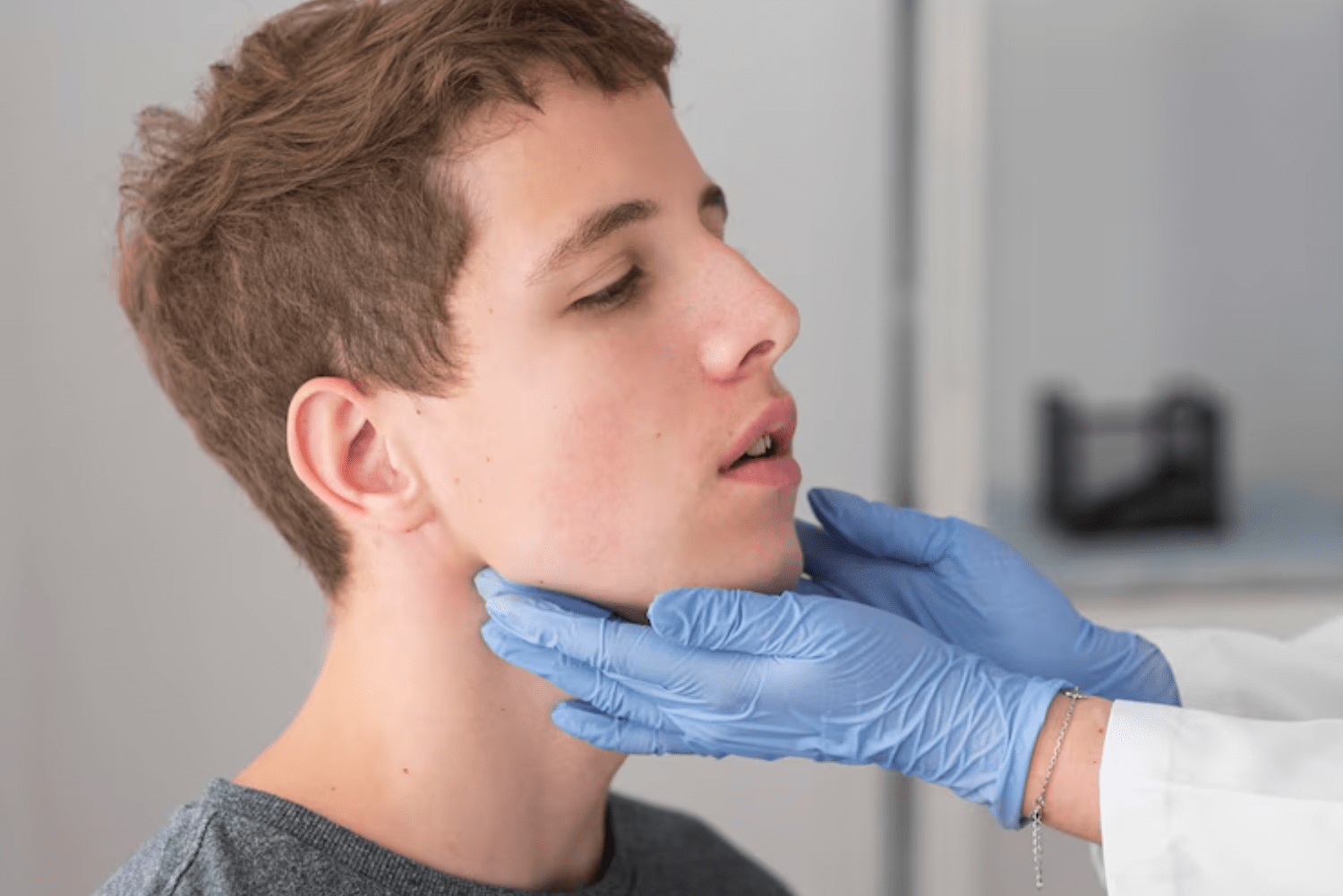
Your healthcare provider will examine you for any broken bone movements on the U-shaped lower jaw. The bruising under your tongue or in the trough of inner lip is suggestive of bleeding between the muscles, usually occurring due to a high-intensity blow on the jaws. Joint movements near the ears are examined. The occlusion is checked. Derangement in the bite is a sign of fracture. All these are part of the clinical assessment for lower jaw fracture treatment.
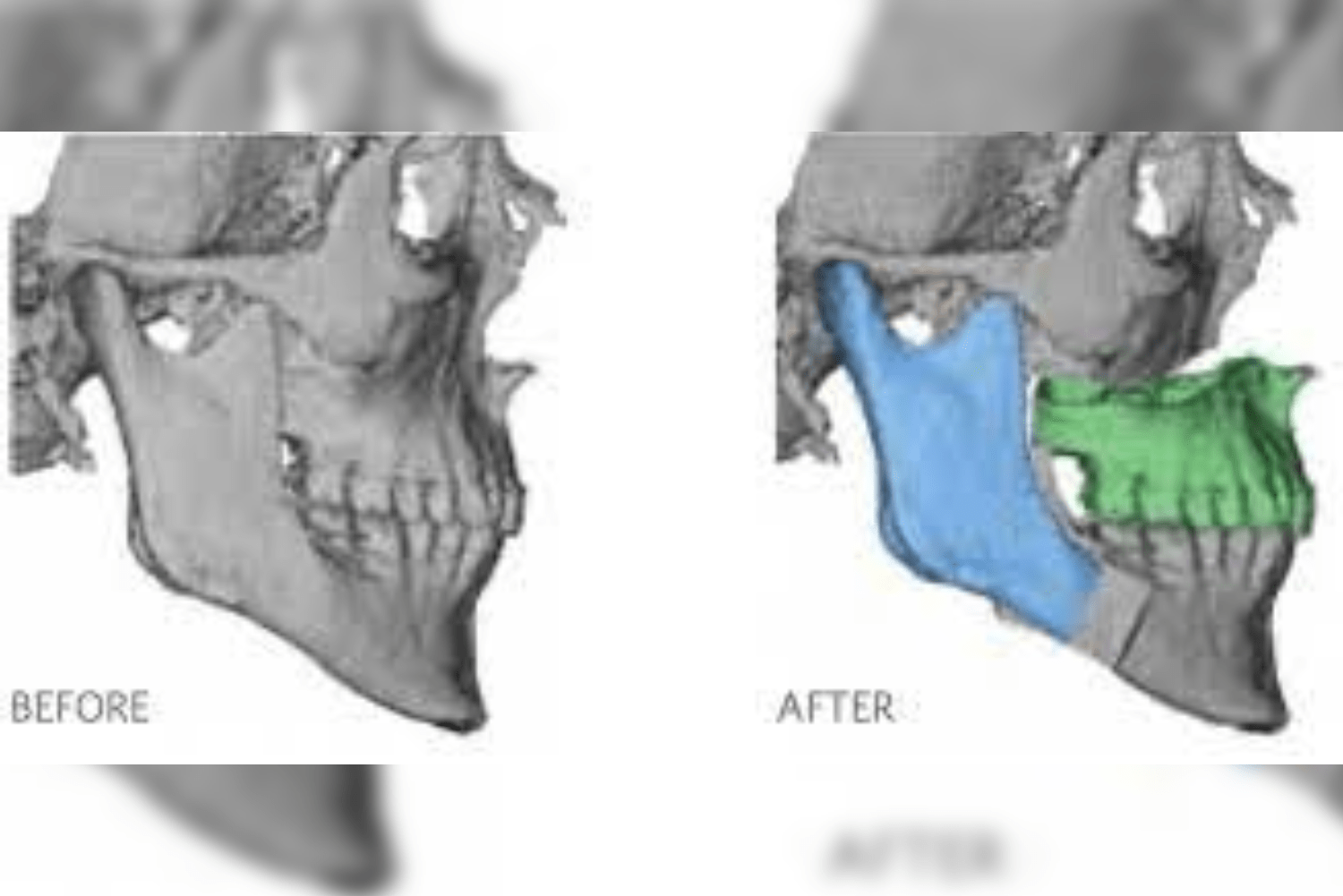
Radiographs like OPG and CT are taken to identify the fracture lines and correlate clinically. The fractures that are displaced are treated surgically by placing titanium plates and screws to stabilize the segments. The teeth may have to undergo wiring to give extra support if needed. These surgical procedures form a critical part of lower jaw fracture treatment.
The fractures that are non-displaced or hairline fractures (greenstick fractures in medical terms) are treated conservatively. An arch bar will be placed around your teeth, suspended by elastics to provide extra support during the healing process. Intravenous antibiotics and analgesics are provided to support healing, whereas oral hygiene plays an utmost importance in the recovery of jaw fractures. During discharge from the hospital, the medication will be changed to oral tablets.
Home Care For Jaw Fracture
Home care of jaw fractures is crucial for the success of lower jaw fracture treatment and includes mainly maintenance of oral hygiene. Once the jaw bones are stabilized using plates or wires, you can start brushing your teeth gently. Mouthwash and chlorhexidine gels will help in wound healing.
Try to avoid sleeping on the side of your jaw fractures. It is always best to sleep straight or in a supine position without any pressure on the fracture site. Proper care at home directly supports the effectiveness of lower jaw fracture treatment.
Do not do forceful rinsing of the mouth as the sutures inside the mouth might get loosened and may require resuturing. Avoid using straws for 2 days, as the negative pressure created inside the mouth while sucking can lead to bleeding. Do not spit forcefully. Apply ice packs on cheekbones or sites of increased pain and swelling. Do not apply heat patches on the fracture site, and avoid rubefacient agents like Zandu Balm or Vicks, as these can worsen healing and cause infection. Follow soft diet advice until advised, and perform mouth opening exercises as instructed by your surgeon to ensure proper recovery after lower jaw fracture treatment.
Diet To Be Followed
Jaw Fracture Diet
Jaw fracture cases undergoing lower jaw fracture treatment are always advised to consume a liquid diet for the first 3 days initially. After the 3rd day, patients can shift to a soft diet. The diet can range from malt to smashed rice or idli. Foods that require minimal chewing are preferred. Make sure your food is not sticky like caramel. Even cakes and ice creams are allowed but shouldn’t contain any jellies or nuts.
2 litres of fluids are a must, which sums up to 10 cups of water or juices if your cup measures 200ml per serving. Hydration plays a major role in healing and recovery after lower jaw fracture treatment. A complete diet includes carbohydrates, fats, proteins, minerals, and vitamins. Three months of multivitamin tablets will benefit in wound healing.
Recommended Foods for Jaw Fracture Patients
-
Soft foods: Foods that can be blended or pureed are easier to consume.
-
Liquid diet: Essential for hydration. Soups and juices hydrate the body while providing essential minerals and vitamins.
-
Nutrient-rich foods: Emphasize protein-rich foods like yogurt, eggs, and pureed meats.
-
Easy-to-chew foods: Opt for soft, tender foods like cooked pasta, oatmeal, scrambled eggs, idli, smashed Pongal, or khichdi to support recovery after lower jaw fracture treatment.
Foods to Avoid
- Hard and crunchy foods: Avoid nuts, chips, or hard candies, chapati, and roti that require a lot of chewing and biting force.
- Sticky foods: Avoid foods like caramel, gum, or dried fruits that can stick to teeth or appliances.
- Spicy or acidic foods: Avoid foods that irritate or cause burning sensations on the tongue, gums or digestive system.
- Hot food: Avoid extremely hot or cold foods that can cause discomfort.
Additional Tips
Eating in small quantities helps in managing discomfort and ensures adequate nutrition. There are no hard rules that your meal timings should be restricted to three times daily. Avoid the use of straws to drink. This causes suction effect leading to negative pressure inside the mouth. This leads to dislodge of clot in the operated site thereby leading to bleeding. These delays healing process. Consult a healthcare professional. An oral surgeon can provide you with personalized dietary plans based on your specific needs and a lower jaw fracture treatment plan. Following these guidelines helps in promoting healing, minimizing discomfort, and ensuring adequate nutrition during the recovery.
Complications Of Jaw Fracture
-
Malocclusion: when the jaw bones are fractures, the teeth present in them can get displaced. Thereby not allowing us to bite properly in occlusion. This is termed as malocclusion. Proper lower jaw fracture treatment helps prevent long-term malocclusion.
-
Infection: when the fracture site is not properly cared, it can lead to infection. The bacteria enter the fracture site, leading to sepsis. Timely lower jaw fracture treatment minimizes the risk of infection.
-
Nerve damage: the nerves passing through the bone can get damaged when the bone fractures. There will be sensory and motor disturbances.
-
Malunion or nonunion: when the jaw bones don’t heal properly, it leads to a mismatch in the original anatomy of the bone. It leads to an increase in pain and restricts the functionality of the jawbone. The bone can also heal with fibrous tissue in between the edges of the fracture without new bone formation. This condition is called a non-union. This leads to mobility in the fracture site.
-
Temporomandibular joint (TMJ) problems: the fracture can lead to a clicking sound in the joint. It can even cause restricted movement of the jaw with severe pain on opening and closing the jaw.
-
Aesthetic concerns: the jaw fractures lead to asymmetry of the face along with scarring of the cut skin wounds. Proper lower jaw fracture treatment can help restore facial symmetry.
-
Difficulty with speech or eating: as the main function of the mouth is to speak and chew food. The fracture in the jaw may hinder these activities.
-
Chronic pain: untreated or partially treated fractures can lead to chronic pain at the fracture site.
-
Limited mobility: a jaw fracture restricts the jaw movements. You will have severe pain when you try to move your jaw. The cut edges of the fracture may override and not allow you to move any bit.
-
Systemic complications: In severe cases, the fracture site might lead to breathing difficulty as the tongue is pushed backward. Also, if the fracture site is infected severely it can lead to sepsis. It’s a major complication where the patient has to be in ICU care and monitored vigilantly to get the infection down.