Mucormycosis is a rare but aggressive fungal infection that can severely affect the face. It is also called black fungus infection.
It affects those with a weak immunity, with conditions like uncontrolled diabetes, post-COVID and those patients on steroids.
Here’s how it affects the face and associated structures step by step:
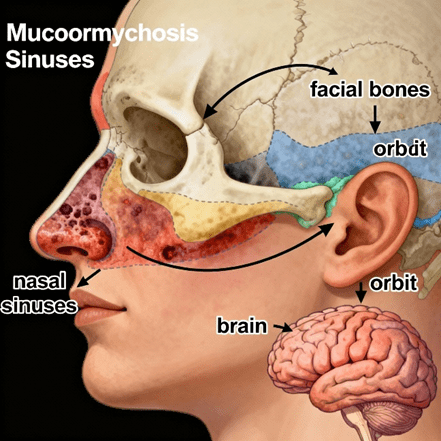
1. Entry and early infection: infection usually starts in the nose or sinuses. This happens by inhalation of fungal spores, commonly Rhizopus mucor and Rhizomucor species. It causes nasal stuffiness or discharge (bloody and black often)
Diffuse swelling around the cheeks, eyes or forehead with Facial pain, severe headache and fever.
2. Spread to facial bones and soft tissues: once the fungus establishes in the facial spaces, it rapidly invades blood vessels until leading to tissue necrosis. That is the death of the cells. This will have an effect on: blackish eschar or discolouration over the nose or palate. Swelling on one side of the face and numbness or loss of sensation due to nerve involvement. Pain and tenderness over the cheek and eye regions.
Affected structures may include: the nasal septum and turbinate with necrosis and perforation.
Osteomyelitis of the maxilla leading to loose teeth and/or facial deformity. Palate ulcers or fistula – a hole connecting the mouth and nose.
3. Orbital and cranial spread – as it progresses, there will be increased periorbital swelling, redness, and pain. Proptosis or bulging of the eyes, loss of vision, restricted eye movements, and facial paralysis when cranial nerves are involved. Cavernous sinus thrombosis or brain invasion, which are life-threatening.
4. Long-term facial effects – even after controlling the infection through antifungal therapy, patients can have: facial asymmetry or deformity, loss of the upper jaw or eye.
It also causes scarring or depression over the cheeks, difficulty in chewing, speaking, and affects facial expressions.
5. Prevention and early detection: it is a mandate to approach doctors to get an evaluation done as soon as possible. Maintain good control of blood sugar, and avoid unnecessary usage of steroids. In case of facial pain, swelling or black lesions, get it immediately evaluated by a maxillofacial surgeon or ENT.
Management of facial mucormycosis:
1. Early detection: Prompt detection is the cornerstone of successful management. A thorough clinical evaluation is made to assess the clinical signs and symptoms.
Unilateral facial pain, black nasal crusting or swelling raises suspicion.
Endoscopic nasal examination: to visualise the inner parts of the nose and to assess necrotic areas.
CT and MRI imaging to scan for bone or soft tissue invasion. Orbital and brain involvement will be detected in the scans.
Biopsy and culture: Oral tissue biopsy is the removal of affected tissue from the site for examination. A culture is a laboratory test that examines the tissue sample for bacteria and other organisms that can cause disease.
Finding the problem early will allow us to initiate the treatment early, thereby avoiding unnecessary progression of the disease.
2. Antifungal therapy: Currently, lipid formulations of amphotericin B have become the standard treatment for mucormycosis due to their efficiency. Once the infection is under control, oral antifungal medicines are continued for several weeks.
As supportive care a strict diabetic control and correction of metabolic acidosis is needed. Steroids and immunosuppressants are discontinued.
3. Surgical debridement: Surgery is a lifesaver I cases of mucormycosis, as medicines alone cannot manage the condition.
- Endoscopic sinus debridement- it removes necrotic tissue from the nasal cavity and sinuses.
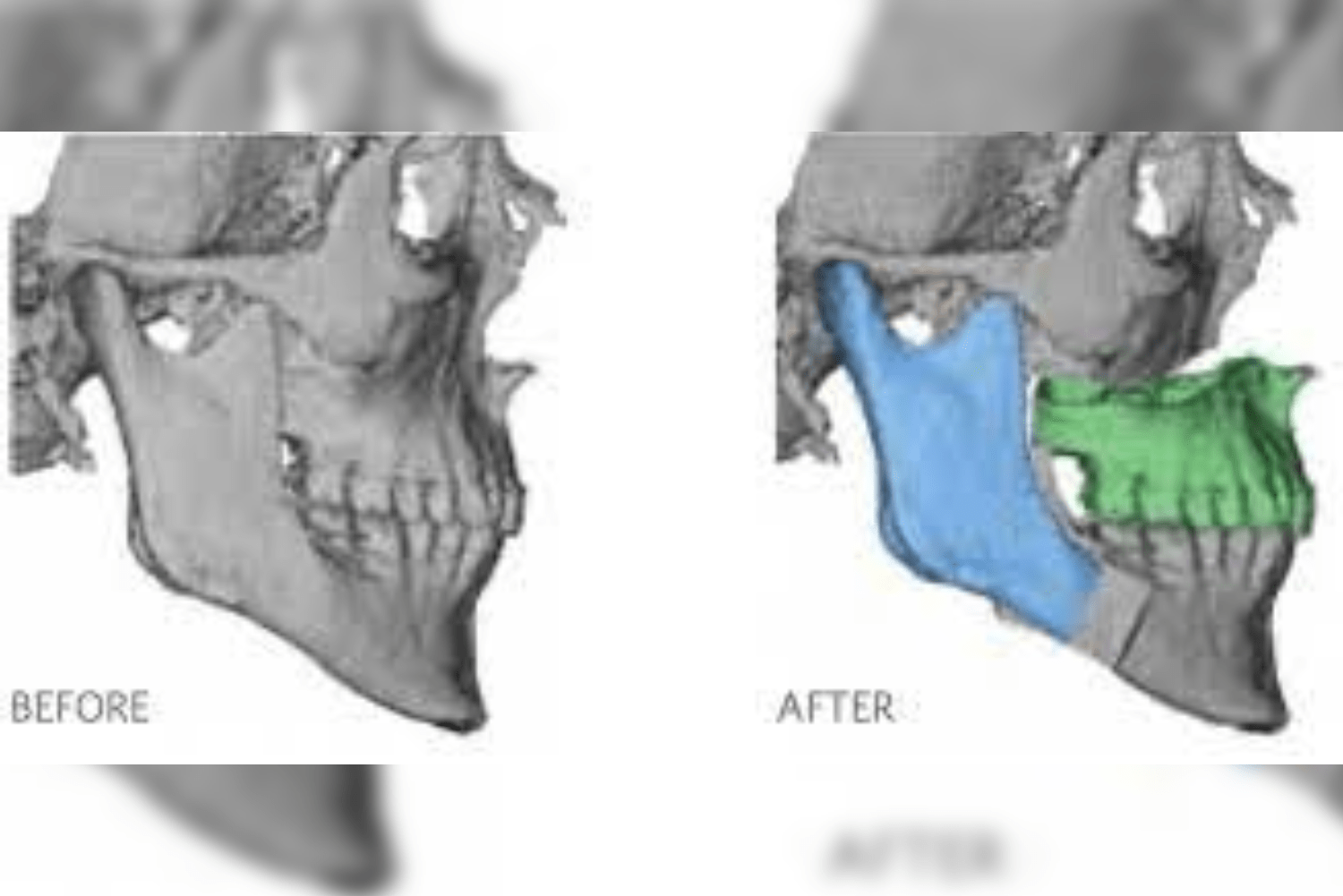
- Maxillectomy- done in cases when parts of the maxilla are infected. The infected part is removed.
- Orbital exenteration- in cases of advanced orbital diseases, the eye is removed. These are performed when vision is lost and infection threatens the brain.
- Palatal debridement- the infected palatal mucosa or bone is removed to prevent to spread of the infection to surrounding structures, even the skull base.
4. Reconstruction and rehabilitation
Once the infection is controlled or free from the disease, the debilitating effects of part or parts of the face removed have to be restored. At Richardson’s face hospitals, we received many patients complaining of a hole in the mouth, connecting the oral cavity to the nose, a hole in the eyes, or in the cheeks.
We came across many types and various cases involving partial loss of face, which needed Reconstruction.
Reconstructive surgery is done after thorough planning.
Free flap Reconstruction: using ALT flap, forearm flap or fibula to rebuild maxilla, orbital or palatal bone.
Bone is grafted from various other body parts to restore jaw continuity and support.
In cases where surgical Reconstruction is not feasible, facial prosthesis and obturators are given.
Dental rehabilitation is done at the last phase using implants or obturator.
Speech therapy is provided to make them have a good speech and swallowing capacity.
Case scenario:
We had a 27-year-old patient who had unfortunately undergone partial Maxillectomy and orbital exenteration a few years back.
He received his dental rehabilitation elsewhere. But never able to close his lips. The exenterated orbit had a fistula, due to which he couldn’t get an eye prosthesis as well.
His only requirement from us was to close the orbital fistula and lengthen the lip. What seemed to be an easy task wasn’t a bit after examination.




His lips were very tight, which had no scope for VY plasty of lips to lengthen it.
The orbital fistula was wide enough with thin surrounding skin, not allowing for direct closure.
We planned a full thickness skin graft to place inside his vestibule to lengthen the lip. To create a rotational flap to provide bulky tissue in the orbit to close it without tension.
And viola it worked and took up great. The patient was discharged in 3 days.
At Richardson Face Hospital, we shall walk along with you in providing the best treatment.