COSMETIC EAR SURGERY
INTRODUCTION Cosmetic ear surgery is a surgery to change the shape, position or size of the ears. This surgery may be used in a number of situations. For example, some people choose to have Cosmetic ear surgery because they are bothered by how far their ears stick out. Others might get this surgery if one or both ears have changed shape due to an injury. Cosmetic ear surgery also may be used if the ears are a different shape because of a birth defect. HISTORICAL BACKGROUND Surgical correction of ear deformities has been reported in the literature as far back as 1845. In the majority of cases, this finding has little relation to other anatomic or physiologic abnormalities. Through the years, hundreds of techniques have been described to correct the auricular deformity. Today, this wide variety of options may hinder the surgeon from choosing the correct procedure best suited for a particular patient. This is why a thorough understanding of ear anatomy is one of the most essential steps in the preoperative management of an Cosmetic ear surgery candidate. With the surgeon’s objective algorithm toward an auricular deformity, the patient may ultimately enjoy the maximal aesthetic outcome possible for his or her case WHO NEEDS IT? The wide range of patients who would benefit from Cosmetic ear surgery are: WHEN IS IT DONE? Once the ears have reached their full size, Cosmetic ear surgery can then be done anytime. Children from 4 to 6 years onwards can get it done. Adults also can get Cosmetic ear surgery. If a baby is born with prominent ears and certain other ear-shape issues, a different treatment may be an option. It’s called splinting, and it doesn’t involve surgery. Devices called splints are placed on the baby’s outer ear. The splints are adjusted each week for about 4 to 6 weeks. For best results, splinting must be done during the first few days of life. This is when the ear is soft and can be molded. Splinting is not proven to be as effective when it’s done after the first few weeks of life. Ear molding/ splinting done for a patient after few weeks of birth to improve ear contour WHY IS IT DONE? You might think about getting Cosmetic ear surgery if: Usually, Cosmetic ear surgery is done on both ears for a balanced look. This concept of balance is called symmetry. Cosmetic ear surgery doesn’t change where on your head the ears are located. It also doesn’t change your ability to hear. TYPES OF COSMETIC EAR SURGERY There are different types of Cosmetic ear surgery, depending on the patient’s needs. Three of the most common are: NON-SURGICAL TECHNIQUES Due to the possible complications of Cosmetic ear surgery, it is important to keep in mind the nonsurgical option when evaluating the prominent ear of an infant. In recent years, splinting has proven to be an alternative option when the prominent ear is detected early after birth. In these cases, correction within the first 96 hours of birth is the most effective. However, the first few weeks of life may still spare the infant from an operative procedure. For optimal correction, bone wax is a reliable material which is commonly used to shape and splint the ear. Surgical tape can be used to cover and hold this in place, and should remain in place for 2 weeks. WHAT TO EXPECT? Before Cosmetic ear surgery can be done in a hospital or in a surgical centre like ours where it is quite frequently performed. It’s usually done under General Anaesthesia where you’ll be given adequate painkillers and antibiotics. During Cosmetic ear surgery techniques vary. The technique your surgeon chooses determines where the incisions are made. There are techniques that make incisions on the backs of your ears or within the inner creases of your ears. Surgeons often choose these areas to help keep Cosmetic ear surgery scars hidden. After making incisions, your surgeon might remove extra tissue including cartilage and skin. Then the cartilage is folded into the proper position and secured with stitches inside the ear. More stitches are used to close the incisions. The surgery typically takes about 1-2 hours. In our centre, we choose the best possible incision design to hide the scar or make it least prominent and/or noticeable. After After Cosmetic ear surgery, your ears will be covered in bandages or dressings for protection from infection and support. Some discomfort and itching is common. The incisions shouldn’t be rubbed or placed force on. A few days after Cosmetic ear surgery, your surgery team removes your bandages. Your ears likely will be swollen. You may need to wear a loose headband that covers your ears at night for a few weeks. This helps keep you from pulling your ears forward when rolling over in bed. Some stitches dissolve on their own. The rest are to be removed by the surgical team in the days to follow after surgery. ADVANTAGES OF COSMETIC EAR SURGERY RISKS AND COMPLICATIONS OF COSMETIC EAR SURGERY As with any surgery, Cosmetic ear surgery has its own fair share of risks. : Results When your bandages are removed, you’ll see a change in how your ears look. These changes are usually are long lasting. If you’re not satisfied with your results, asking your surgeon if a second surgery is worth it would help. This is known as a Revision surgery. RECOVERY AND OUTLOOK What is the recovery time? Cosmetic ear surgery recovery can take up to eight weeks. Improvements are visually noticeable in two to three weeks. Healing times may vary for everyone. What about follow-up appointments? Your surgeon wants to know if your ears are healing well. The first follow-up is usually 1 week after the surgery. Here, they’ll remove your dressing/bandages. After that, you need to see your surgeon for one to two more follow-ups over the next few weeks to ensure that healing is in progress and your recovery is on track. CONCLUSION Our
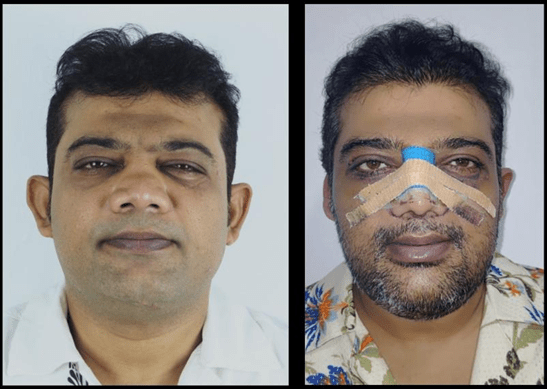
Breathing Better, Looking Better: Understanding Functional Nasal Reconstruction

Functional nasal reconstruction, also known as functional rhinoplasty, is a surgical procedure used to correct breathing problems. It is done by reshaping and repositioning the structures inside and outside the nose. Several people have an obstructed or stuffy nose most of the time. The conventional treatments, like steam inhalation or medication, would not solve the issue. The underlying issue has to be diagnosed priorly there is prolonged period of nasal obstructions. Most often, we have come across people suffering from breathing difficulty that would have led to sleep disturbances, an increased number of headaches, unable to work, disturbed concentration, daytime snoring, etc. All of these issues are commonly related to problems with breathing patterns. Cosmetic rhinoplasty is performed for the aesthetic improvement of the nose. This involves changing the size, width, shape, breadth, tip projection and angulation of the nose and also the creation of the dorsal aesthetic line. Rhinoplasty is a surgery of millimetres. At Richardsons, we provide the best rhinoplasty treatment in India. With over 10,000 cases of experience, both in India and abroad, Dr Sunil Richardson is equipped to deliver the noses of your dreams. The main reasons for having difficulty in breathing will be due to a deviated nasal septum, enlarged nasal turbinate or nasal valve collapse that can cause obstruction. The functional nasal reconstruction surgery can be performed along with cosmetic rhinoplasty to improve the appearance simultaneously. The common surgical techniques used in the nose surgery are septal reconstruction and septoplasty to straighten the septum, and spreader grafts or alar batten grafts to widen the nasal passages or valves. What is this procedure? Functional surgery of the nose is a surgical procedure to improve nasal breathing. It can also be combined with cosmetic rhinoplasty to improve the aesthetic profile of the nose. It mainly addresses the functional breathing difficulties that can be due to trauma, congenital or birth defects or due to previous surgery. What does it treat Deviated nasal septum: our nose is divided by a cartilage and bone that is called the septum. When this wall between the nostrils isn’t straight, breathing will be difficult. Deviated nasal septum. Observe the deviation towards the left in the centre septum. Observe the S-shaped bend of the nasal septum towards the left. Nasal valve collapse: the nose has 2 valves. external valve and internal valves. It is the opening of the nostril that you see. When these valves are collapsed, the nose appears pinched up in the tip region, particularly during inhalation. Nasal valve collapse Large turbinates: these are curled bony structures in the sides of the nose. These are present inside the nose. They warm, humidify, and filter the inhaled air. They are present in 3 pairs, called the superior, middle and inferior turbinates. The inferior turbinates are the largest of all and most likely swell due to allergies or infections. This condition is known as turbinate hypertrophy. This creates nasal obstructions and difficulty in breathing. Other issues: other problems like chronic sinus infections, nasal injuries, fractures and certain congenital defects or septal wall perforation are the reasons for nasal obstructions and difficulty in breathing. How are they corrected surgically? A small incision is made inside the nose, and the cartilage is repositioned, and the bony deviations are removed. This will heal normally with some swelling and bleeding takes about one to 2 weeks of recovery. 2. Spreader grafts: This is a type of graft that will be placed alongside of the nasal septum to increase the size of the internal nasal valve area. The craft will be taken from the patient’s own body. It is a small piece of cartilage that will be harvested from the rib cartilage, the ear cartilage, or the patient’s own remaining nasal septum. This helps in keeping the nasal septum straight as well, by providing extra support. Rib graft is an autologous graft that is harvested from the patient’s own body. It involves harvesting the rib cartilage from the rib cage, and it is used to augment or reconstruct the framework of the nose. 3. Alar batten grafts: These are the small cartilage species that are placed inside the ala. This increases the rigidity and support of the side walls of the nose. When the support has increased, it prevents the collapse of the nose during inhalation. Any nasal asymmetry that is due to the difference in the alar thickness will be corrected using this method. Reconstructive rhinoplasty: This type of nose job is performed when major reconstructions are needed on the nose, often following road traffic accidents, major cancer or tumour surgeries, or even after multiple failed previous nose surgeries. These procedures can involve reconstructing the bony architecture of the nose as well as addressing overlapping soft tissue. The deviation of the nasal tip pointing towards right before surgery(right). This was corrected with surgery (left). Benefits of this surgery The benefits of this surgery are : 1. You can notice improved airflow and breathing, especially during sleep or exercise. 2. Symptoms like mouth breathing, dry mouth and exercise intolerance will be resolved. 3. Potential issues like chronic sinusitis and headaches that would cause disturbance in daily lifestyle would be corrected. 4. It is a functional surgery, but cosmetic rhinoplasty can also be performed along with this at the same time. This offers aesthetic goals, so patients can achieve both better breathing and improved appearance. 5. Rhinoplasty or nose correction surgery’s results usually last for a lifetime with little to no change at all. But certain factors, such as the natural ageing process or an accident, may result in slight alterations to your nose. 6. Dr Sunil Richardson has helped many patients resolve the issue of their snoring through Functional Rhinoplasty Surgery, and has brought a smile to each and every patient. What is the course of events that you undergo at Richardson’s Face Hospital? On your visit to the hospital, you will be consulted in our outpatient department. 3d CBCT scans are taken to analyse the underlying
Everything to know before Blepharoplasty

Blepharoplasty is a surgery done to enhance or improve the eyelid appearance. It is aimed at making the eyes appear bigger by removing the droopy skin around the eyes. But sometimes it might just be as little as repositioning the fat around the eyes. This procedure removes baggy eyelids and smooths the eyelid contours. Do you need blepharoplasty? It is a simple answer. It is for those who want to lift their eyes, those who have baggy eyelids, excessive wrinkles and droopy eyelids. Among other criteria include: Patients who are usually over 45 years old seek blepharoplasty. But it can be beneficial to the younger generation who have a genetic predisposition of droopy and baggy eyelids. Though there are no absolute contraindications for the surgery, certain conditions of the eye like: Before opting for the procedure, many patients’ only concern is how safe it is to undergo the procedure with these underlying systemic issues. For that, always talk to your surgeon and discuss the safety concerns. How is this procedure performed? This procedure is performed by removing the excess amount of skin and fat present underneath the eyelids. It can be performed either under local or general anaesthesia. A simple blepharoplasty involves the removal of an excessive amount of skin and fat can be performed under local anaesthesia. Whereas a procedure that has extensive removal of fat and repositioning of orbital muscles requires general anaesthesia. This procedure can also be performed with other procedures like browlift, facelift, rhinoplasty, etc. There are 2 types of blepharoplasty.: 1. Upper blepharoplasty 2. Lower blepharoplasty This is a surgery performed on the upper eyelid to remove excess amount of skin, fat and correct drooping of the lids. this helps in providing good contour to the upper eyelid as well as removing the hooding of the eyelid. An excessive amount of skin and fat is removed and tightened. This will improve the lateral vision of patients having excessive hooding of eyes. This procedure creates a smooth eyelid crease line. It also removes excessive wrinkles on the corners of the eyes called crow’s feet. Surgery on the upper eyelids generally involves: Closing the incision – the scar will usually be hidden in the natural fold of the eyelid. 2. Lower blepharoplasty: It involves removing or repositioning of excessive amount of skin, fat and muscle in the lower eyelid, which reduces the puffy appearance below the eyelids and also reduces the dark circles. This type of surgery mainly aims to improve the overall appearance of the lower eye area. Just as said in upper eyelid surgery, lower eyelid surgery also utilises the natural crease lines. Surgery on the lower eyelids generally involves: The surgeon will usually apply thin, sticky strips called suture strips to support the eyelids after surgery. These are usually removed up to 1 week later. Eyelid surgery may take around 45 minutes to 2 and a half hours. Most people can go home the same day. Pre operative evaluation Preoperative patient evaluation for blepharoplasty should document medical and ophthalmologic history such as chronic systemic diseases and medications. Ophthalmologic history should be obtained, including vision, corrective lenses, trauma, glaucoma, allergic reactions, excess tearing, and dry eyes. No cosmetic surgery of the periorbital region should be performed for a minimum of six months following corneal refractory surgery. How should one prepare for a Blepharoplasty? What are the risks of Blepharoplasty? It is common to have these signs after your blepharoplasty surgery, : These are all temporary, and with time and a few weeks of rest and care, they resolve. Blepharoplasty recovery Recovery of blepharoplasty is very short compared to other cosmetic procedures. This procedure is mainly a day-care procedure that doesn’t even require a hospital stay. There might be sutures along the incision line, which will be removed after a week’s time. In cases where absorbable sutures are used, these sutures need not be removed. In post postoperative period, you may experience : These, however, will resolve with post-op care and medications. The bruising might be present for 1–2 weeks. The suture marks gradually fade away and might take a month. For an easy recovery, your surgeon may advise you to follow these instructions: Mild bruising and redness around the eyes and inside the eyes will take 2-3 weeks to disappear. Patients are advised to avoid strenuous activities, exercises, heavy lifting and bending over for at least one week to reduce the risk of bleeding and swelling. eyes should be protected from the sun and wind by wearing sunglasses. The lubricating eye drops provided are recommended by the surgeon and it aids in easy and faster recovery. How long do these results stay? While blepharoplasty improves the natural texture, smoothness and crease line around the eye, it will not stop the natural ageing process. This surgery results last for several years, but is not a permanent result. The person undergoing this procedure looks ten to fifteen years younger. But as the ageing process, new wrinkles may form while the existing wrinkles and puffiness will all be removed. The best ways to preserve and regenerate the skin are by : Scarring on the eyelids after blepharoplasty? Out of so many cosmetic procedures available on face, the incisions planned for blepharoplasty are the best ones. It is because the incision is always given on the crease lines already existing and scars are always inconspicuous. Depending on the type of surgery that is planned for you, the incision is planned. This allows and ensures that postoperatively, there are no visible incision lines. There is generally little or no evidence of incisions after complete healing. It is also important to take care of the wound healing after the surgery very diligently. This encourages the scar to lighten and become even more discreet over time. At Richardson Face Hospitals, we have professionals to take care of your eyelids like no one else. Will there be any vision improvement after the procedure? Blepharoplasty is mainly a cosmetic surgery, so it has no
ROLE OF TEETH CLEANING AND GOOD BRUSHING FOR ORAL HYGIENE
The basics of good oral hygiene are always maintaining a proper brushing habit and visiting your dentist regularly. But brushing alone does not aid in good oral hygiene. A proper general dental visit should be done once every six months. So that any kind of dental issues can be identified and treated in the early stage itself. TIPS FOR DAILY CARE FOR THE TEETH: ADVANTAGES OF TEETH CLEANING: MYTHS AND TRUTH ABOUT TEETH CLEANING: TRUTH: Scaling only removes the extra deposit, plaque, and calculus in your teeth. It will not any harm to the teeth TRUTH: Scaling will not be painful at all. We have modern equipment in our Richardsons Face Hospital. Through which the dental scaling can be done pain-free and the patient will be more comfortable. If they still feel pain or sensitivity, can be treated by applying local anesthetic agent or a desensitizing paste, which can be helpful to the patient. TRUTH: Scaling will not lose or weak your teeth and gums. If the are more deposits and they didn’t maintain their oral hygiene well can leads to mobility of the teeth. For that kind of individuals, once the scaling done, minimal tooth mobility will be there, which can be treated by giving the mouthwash, gum paint and proper follow-ups TRUTH: It will not create any spaces in between the teeth. If you think so, it’s usually because of the deposits or calculus which was already built in between your teeth, which got removed by the dental scaling. TRUTH: Sensitivity after dental scaling is temporary. After scaling, teeth and gums take little time for the adaptation. It will get normal within three days of time. TRUTH: Dental cleaning will not whiten your teeth. It will remove your deposits and calculus. The polishing of your teeth can remove the stains which are extrinsic. But still, it will not whiten your teeth. WHAT WILL DENTIST DO IN SCALING: POST INSTUCTIONS AFTER SCALING: BRUSHING TECHNIQUE: FLOSSING TECHNIQUE: IMPORTANCE OF FLOSSING: HOW TO DO FLOSSING: OBSTACLES TO MAINTAIN GOOD ORAL HEALTH: CONCLUSION:
BEARD TRANSPLANTATION SURGERY
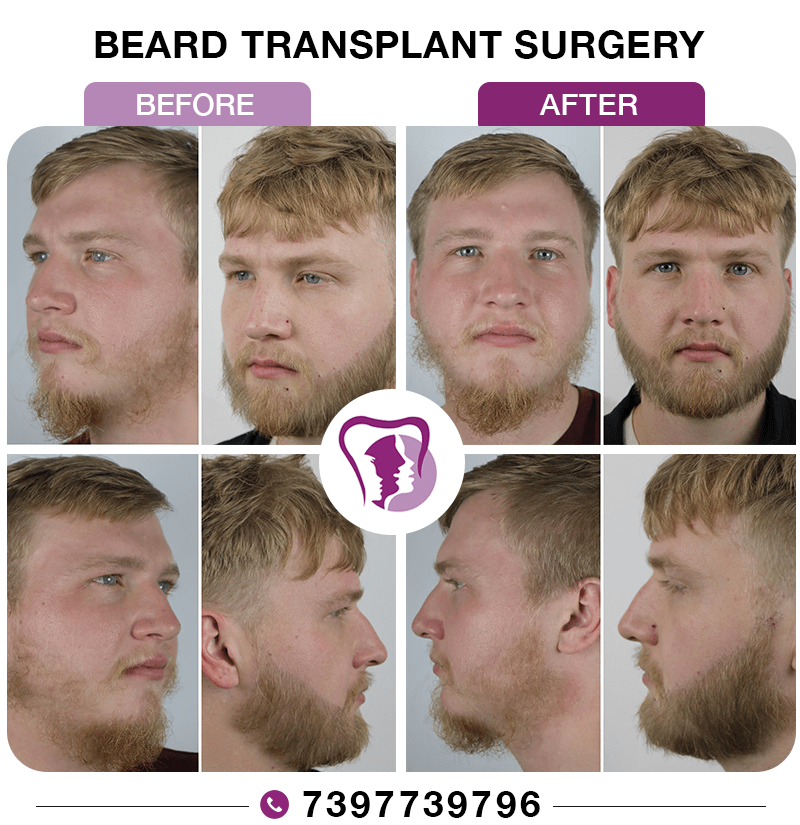
Introduction: Beard transplant surgery involves extracting hair follicles from a donor site and then transplanting them to the beard area. This is a special form of hair transplant surgery A permanent, natural-looking beard is usually achieved with such surgeries that can be trimmed and styled like natural facial hair. The techniques used for the beard transplant are: In the Follicular Unit Transplantation (FUT) technique, a thin strip of scalp is removed and stripped into multiple individual follicular units. In the Follicular unit extraction (FUE) technique, individual follicles are extracted using punches that are sized around 0.8mm-1mm, and are implanted directly into the beard area. Clinics today primarily use the FUE method, as it leaves minimal to no scarring and ensures faster recovery. It also allows for artistic customization of the beard shape and density. Who benefits from it? Beard transplantation isn’t limited to cosmetic enhancement. It also serves a reconstructive purpose for patients recovering from illness, injury, or surgery. Indications include: Genetic factors and hormonal imbalances can cause uneven beard growth. A beard transplant helps fill in these gaps. Burns and facial scars can destroy beard follicles. After head and neck cancer surgery or radiation therapy, patients often lose their facial hair. They even develop scarred areas on the face. In such cases, beard transplantation helps mask these regions Thus, it aids in emotional recovery by restoring self-confidence to the patient. It is indicated for men who desire a fuller goatee and sideburns or even a denser beard that enhances their looks. Preoperative evaluation and planning -Donor hair quality, density, texture, curl -Beard design and symmetry -Skin condition and vascularity -Patient expectation and esthetic goals Inside the operating theatre with the entire team Step One: Anaesthesia and preparation The team members involved are: Surgeon– Leads and performs the key steps. Nurses and assistants– Prepare the patient and assist throughout the procedure. Technicians– Handle follicles under magnification. Anesthetist- Monitors comfort and vitals if sedation is used. Step Two: Donor hair extraction Step Three: Designing the beard Step Four: Creating the recipient’s site Step Five: Graft implantation Step Six: Final dressing and recovery How long does a beard transplant procedure take? It’s typically performed as a day care procedure under local anaesthesia Recovery and aftercare Proper aftercare is essential for graft survival and optimal growth First few days: Two weeks: One to Three Months: Six-Nine Months: Nine- Twelve Months: The surgical team behind every successful beard transplant The coordination of a dedicated, efficient multidisciplinary team is required to get a seamless beard transplant procedure. Team Member Role Hair Restoration Surgeon Prepare grafts, manage equipmen,t and support patient care Assistants / Nurses Prepare grafts, manage equipment and support patient care Technicians Handle follicles under microscopes to maintain graft integrity Anesthetist / Sedation Expert Ensures comfort and safety throughout the procedure Support Staff Maintain sterility and theatre efficiency Every graft placed represents teamwork, precision, and attention to detail. Quick Summary Parameter Details Procedure Time 6–8 hours (day-care surgery) Anesthesia Local (with or without sedation) Technique FUE / FUT Downtime 2–3 days Visible Results 6–12 months Longevity Permanent Ideal Candidates Men with sparse beards, post-trauma scars, post-cancer recovery, or gender affirmation Complications When performed by experienced surgeons in accredited facilities, beard transplants are extremely safe. Possible but rare side effects include: Beard transplant in post-cancer and post-traumatic cases For patients with facial scarring due to burns, trauma, or cancer surgery, beard transplantation plays a reconstructive role. However, these require special considerations: The results can be life-changing, helping patients camouflage scars, restore symmetry, and rebuild confidence after illness or injury. Results and Longevity Transplanted beard hair behaves like natural hair, and it can be shaved, trimmed, or styled just like how it grows as natural hair. Since they originate from the permanent donor zone, they continue to grow for life. No special maintenance is required beyond regular grooming. Here, in the pictures shown below, we have a patient who flew all the way from Canada to our hospital with a chief complaint of sparse hair over his beard region that he attributes to a traumatic injury in childhood. A pre-operative evaluation of the hair density and texture was done along with the routine blood investigations and systemic evaluation for the procedure. After obtaining fitness for the procedure, he was taken up for a beard transplantation. The before and after photographs show his transformation, where scanty hair is now replaced with a full crop of hair, giving him a defined, chiseled, masculine look.
DENTAL EMERGENCIES

A dental emergency is a situation that requires immediate attention from a dentist to reduce severe pain, prevent further damage, or save a tooth. There are two categories of dental emergencies A.Common dental emergencies These are 1. Severe toothache: Intense pain or swelling in the tooth or surrounding area, or severe orofacial trauma 2. Trauma: Injury to the vital teeth, mouth, or gums 3. Knocked-out tooth: Tooth is completely avulsed from the socket 4. Broken or chipped tooth: Trauma to a tooth 5. Infection: acute apical abscess, irreversible pulpitis, or severe dental caries Acute pain is generally time-limited and responsive to pharmacotherapy or direct intervention. Examples of conditions known to cause chronic pain in a dental setting are The immediate attention to the cause is necessary when treating emergencies; these are Procedures: NON-PHARMACEUTICAL THERAPIES FOR DENTAL PAIN: PHARMACEUTICAL THERAPIES FOR DENTAL PAIN The most commonly prescribed drugs for dental pain in our hospital are All the above-mentioned drugs are given through the oral route. For children, the dosage is calculated according to body weight, and usually paracetamol is given through the oral route in the form of syrup. The maximum dosage of paracetamol per kg body wt. is 10-15mg/kg body weight. Based on the pain intensity, the syrup can be given 3-4 times daily. The paracetamol syrup is available in two concentrations: 125mg/5 ml and 250mg/5 ml. The dosage of the oral medication is decided depending on the patient’s intensity of pain, severity of the condition, and the patient’s accompanying medical conditions. B.On chair dental emergency “On chair dental emergency” is a situation where a patient experiences a dental emergency while already undergoing dental treatment on the dental chair Possible Scenarios 1. Sudden pain or discomfort: Patient experiences unexpected pain or discomfort during a procedure 2. Tooth fracture or breakage: Tooth breaks or fractures during treatment 3. Instrument breakage: Dental instrument breaks or gets stuck in the patient’s mouth 4. Allergic reaction: Patient has an allergic reaction to a medication or material used during treatment The most common medical emergencies that can occur in a dental chair are ASTHMA Signs and Symptoms: Wheezing when exhaling, coughing, and shortness of breath Treatment Precautions: • Make sure the patient has their medication with them at the time of the appointment • For controlled asthmatics, LA with Epinephrine should be used judiciously; this is because the sulphite used as a preservative may bring about an allergic attack. • Agree on a signal for distress with the patient before beginning treatment • Avoid Aspirin or NSAIDS Treatment: • Have the patient signal you that they need their medication • Have the patient administer their own medication (bronchodilators) • Deriphyllin (i.v.) and Salbutamol inhaler are to be given • Administer Oxygen if deemed necessary EPILEPTIC SEIZURES Signs and Symptoms: • Patient may have a previous history of seizures • Patient may recognize they are coming by a preceding “aura” • Altered consciousness levels • Muscle rigidity • Convulsions • Apnea (temporary absence or cessation of breathing) • Cyanosis Treatment Precautions: • If the patient usually recognizes when seizures are about to happen, discuss a signal they can give about an impending seizure • Make sure the patient has taken their medication that day • Have Oxygen Ready • Be prepared to remove the clamp, rubber dam in case of an episode of seizures. Treatment: • Place the patient on his side on the floor away from objects until the seizure subsides • If the patient vomits, suction • If seizure lasts longer than 5 minutes, call for Emergency Medical Services • Administer Oxygen if deemed necessary ANAPHYLACTIC SHOCK/ ALLERGIES Signs and Symptoms: • Respiratory distress, wheezing • Airway obstruction • Rapid, weak pulse • Palpitations • Swelling of lips or eyelids, eyelids may itch and tear • Difficulty swallowing • Nausea and vomiting • Urticaria (hives) Treatment Precautions: • Always perform a complete medical history to reduce the likelihood of an allergen exposure Treatment: • Call EMS immediately • Administer epinephrine • If pulse present, elevate legs, give oxygen • If no pulse or breathing, begin CPR • If the patient vomits, suction • Continue CPR or monitor vital signs until EMS arrives DIABETES Elevated glucose levels in blood and urine. Persons diagnosed with Diabetes may suffer from too high or too low blood sugar at times, depending on medications, food intake, illnesses, or stress. Signs and Symptoms: Hypoglycemia Rapid onset –within minutes, Nervousness, Pallor, feeling Weak and dizzy, Hunger, nausea, Mental confusion, Lethargy, Decreased rate of breathing, Increased heart rate, Decrease in blood pressure, Seizures, Tingling sensation in feet/hands, Loss of consciousness. Hyperglycemia Slow Onset – hours or days, feeling Hot and dry, flushed malaise, Nausea and vomiting, Stupor, Drowsy, Irritability and Headache, Acetone odor, decreased blood pressure, increased heart rate Treatment Precautions: • Ensure the patient has eaten and has had their medication before the appointment • Keep appointments short • Have a sugar supplement on hand Treatment: • If conscious and able to swallow well, give a sugar supplement. Call for Emergency Medical Services if the patient doesn’t feel better in 15 minutes or becomes unconscious. • If unconscious, call Emergency Medical Service immediately SYNCOPE Temporary loss of consciousness with inability to maintain postural control Causes: • Fear, pain, or stress • Fatigue • Overly warm environment • Decreased blood flow to the brain, vasovagal event Signs and Symptoms • Restlessness • Pallor • Feeling “too warm” • Cold and clammy skin • Nausea, generally feeling unwell • Breathing may be irregular • Slow, feeble pulse • Convulsive movements, twitching • Loss of consciousness Treatment: • Lay patient in a horizontal “head below feet” position • Loosen tight clothing • Monitor ABC’s (Airway, Breathing, and Circulation) • Ask the patient to smell a cotton pledget soaked in spirit of ammonia (respiratory stimulant) • Give Oxygen if required • Call for emergency medical services if the patient does not recover within 10 minutes MYOCARDIAL INFARCTION Signs and symptoms • Chest pain of pressure. •
Fighting Mucormycosis: Early And Later Care To Restore The Face.

Mucormycosis is a rare but aggressive fungal infection that can severely affect the face. It is also called black fungus infection. It affects those with a weak immunity, with conditions like uncontrolled diabetes, post-COVID and those patients on steroids. Here’s how it affects the face and associated structures step by step: 1. Entry and early infection: infection usually starts in the nose or sinuses. This happens by inhalation of fungal spores, commonly Rhizopus mucor and Rhizomucor species. It causes nasal stuffiness or discharge (bloody and black often) Diffuse swelling around the cheeks, eyes or forehead with Facial pain, severe headache and fever. 2. Spread to facial bones and soft tissues: once the fungus establishes in the facial spaces, it rapidly invades blood vessels until leading to tissue necrosis. That is the death of the cells. This will have an effect on: blackish eschar or discolouration over the nose or palate. Swelling on one side of the face and numbness or loss of sensation due to nerve involvement. Pain and tenderness over the cheek and eye regions. Affected structures may include: the nasal septum and turbinate with necrosis and perforation. Osteomyelitis of the maxilla leading to loose teeth and/or facial deformity. Palate ulcers or fistula – a hole connecting the mouth and nose. 3. Orbital and cranial spread – as it progresses, there will be increased periorbital swelling, redness, and pain. Proptosis or bulging of the eyes, loss of vision, restricted eye movements, and facial paralysis when cranial nerves are involved. Cavernous sinus thrombosis or brain invasion, which are life-threatening. 4. Long-term facial effects – even after controlling the infection through antifungal therapy, patients can have: facial asymmetry or deformity, loss of the upper jaw or eye. It also causes scarring or depression over the cheeks, difficulty in chewing, speaking, and affects facial expressions. 5. Prevention and early detection: it is a mandate to approach doctors to get an evaluation done as soon as possible. Maintain good control of blood sugar, and avoid unnecessary usage of steroids. In case of facial pain, swelling or black lesions, get it immediately evaluated by a maxillofacial surgeon or ENT. Management of facial mucormycosis: 1. Early detection: Prompt detection is the cornerstone of successful management. A thorough clinical evaluation is made to assess the clinical signs and symptoms. Unilateral facial pain, black nasal crusting or swelling raises suspicion. Endoscopic nasal examination: to visualise the inner parts of the nose and to assess necrotic areas. CT and MRI imaging to scan for bone or soft tissue invasion. Orbital and brain involvement will be detected in the scans. Biopsy and culture: Oral tissue biopsy is the removal of affected tissue from the site for examination. A culture is a laboratory test that examines the tissue sample for bacteria and other organisms that can cause disease. Finding the problem early will allow us to initiate the treatment early, thereby avoiding unnecessary progression of the disease. 2. Antifungal therapy: Currently, lipid formulations of amphotericin B have become the standard treatment for mucormycosis due to their efficiency. Once the infection is under control, oral antifungal medicines are continued for several weeks. As supportive care a strict diabetic control and correction of metabolic acidosis is needed. Steroids and immunosuppressants are discontinued. 3. Surgical debridement: Surgery is a lifesaver I cases of mucormycosis, as medicines alone cannot manage the condition. 4. Reconstruction and rehabilitation Once the infection is controlled or free from the disease, the debilitating effects of part or parts of the face removed have to be restored. At Richardson’s face hospitals, we received many patients complaining of a hole in the mouth, connecting the oral cavity to the nose, a hole in the eyes, or in the cheeks. We came across many types and various cases involving partial loss of face, which needed Reconstruction. Reconstructive surgery is done after thorough planning. Free flap Reconstruction: using ALT flap, forearm flap or fibula to rebuild maxilla, orbital or palatal bone. Bone is grafted from various other body parts to restore jaw continuity and support. In cases where surgical Reconstruction is not feasible, facial prosthesis and obturators are given. Dental rehabilitation is done at the last phase using implants or obturator. Speech therapy is provided to make them have a good speech and swallowing capacity. Case scenario: We had a 27-year-old patient who had unfortunately undergone partial Maxillectomy and orbital exenteration a few years back. He received his dental rehabilitation elsewhere. But never able to close his lips. The exenterated orbit had a fistula, due to which he couldn’t get an eye prosthesis as well. His only requirement from us was to close the orbital fistula and lengthen the lip. What seemed to be an easy task wasn’t a bit after examination. His lips were very tight, which had no scope for VY plasty of lips to lengthen it. The orbital fistula was wide enough with thin surrounding skin, not allowing for direct closure. We planned a full thickness skin graft to place inside his vestibule to lengthen the lip. To create a rotational flap to provide bulky tissue in the orbit to close it without tension. And viola it worked and took up great. The patient was discharged in 3 days. At Richardson Face Hospital, we shall walk along with you in providing the best treatment.
Facial Burn Injuries: Treatment Beyond The Depth Of Burns

Burn injuries are a significant health issue and are a leading cause of accidental death or injury in India. Burns to the face can affect many specialised structures that are critical to survival and human function to include the mouth, nose, eyes, and ears. Beyond the functional aspect of facial burns, the aesthetic component is critical as we interact with the rest of the world with our faces. Contractures and hypertrophic scars are two frustrating sequelae of thermal injury. Scars of the face and neck region are prone to be unusually severe because: 1. Its skin is rather loose, thin and thus easily destroyed 2. The area from the chin to the sternum is a concave flexor surface. 3. The extreme mobility of the neck makes it prone to contracture formation. 4. Vertical incisions in the skin of the anterior cervical area, whether accidental or surgical, are likely to result in contracted scar bands. Other than burn scar and contracture, these patients are completely healthy and successful reconstructive surgery can often restore them to a happy and productive life. Patience, persistence, and determination are essential to accomplish successful reconstruction. The ultimate principle of reconstruction of post-burn neck contracture is learning to understand, appreciate and favourably influence the process of wound healing & scar maturation. Patients with facial burns present the clinician with the challenge of treating both functional and aesthetic needs. At its most basic, the face is needed for breathing and oral intake. It is also remarkably complex in its anatomy, providing us with sight, hearing, and smell. Facial burns have many long-term physical, psychological and social sequelae. They require a healthcare team approach to management, which could last months to years. Burns injuries can be the result of thermal (flames, hot liquid, contact with hot surfaces), or non-thermal (electrical, chemical, friction or radiation) contact. The treatment of facial burns aims to: If a patient is able to comply with physiotherapy and occupational therapy advice in the long-term, this can make a huge difference to the overall outcome. The skin in made up of a number of layers: A first-degree burn damages the epidermis, a second-degree burn will also damage the dermis layer, and a third-degree burn is deep and damages the subcutaneous tissue. The depth of the burn will affect the risk of skin pigmentation, risk of scarring and also the length of time to heal. Healing Timeframes Post-Burn Injury Table adapted from Glassey 2004 Degree MOI Scar / contracture 1st Sun exposure, hot liquid (low viscosity) None 2a (superficial) Hot liquids, chemical burns, flash Minimal 2b (deep) Flame, electrical, hot liquid (high viscosity) High risk 3rd Flame, electrical, chemical, blast Severe risk 4th Prolonged exposure to flame, chemical, blast Definite Oedema: Your face and neck are at high risk of burns, as it is rarely covered by clothing or other protective gear. However, there are protective characteristics that often reduce the depth of burn injuries to these areas : Widespread complications of deep or widespread burns can include sepsis due to loss of barrier to infection, burn shock due to hypovolemia, vascular resistance, hypoperfusion and anti-inflammatory processes, as well as contracture due to formation of scar tissue. Burns can also lead to dehydration due to a loss of bodily fluids due to the death of skin cells. Risks by area The risks for body areas are: Back of head: Area of thin skin with risk of exposure of underlying bone. It may also result in areas of alopecia. Ears: Risk of exposure of the underlying cartilage, which is relatively avascular and at risk of infection. Forehead: Less fat and muscle in this area can increase the risk of exposed bone. Eyelids: Also thin skin and at risk of exposure of underlying tissue/eyeballs. They also provide little resistance to forces of contracture and are prone to forming ectropions, exposing the inner eyelid. Eyes: Ocular burns may lead to infection or tissue ischemia. Chemical burns, particularly to the cornea, are an ophthalmologic emergency. Nose: Risk of shrinkage of the nostrils and the nasal alae. Also at risk of exposure of underlying cartilage and bone, which are relatively avascular and at risk of infection. Singed nasal hairs may indicate inhalation injury. Cheeks: This area has mobile, thick skin with good resistance to skin contracture. However, difficult to immobilise for healing post-surgery. Lips: Prone to shrinkage or eversion as a result of contractures. Significant swelling of the lips or tongue may compromise the airway. Neck: More prone to contractures in younger patients, due to reduced laxity. The skin loosens with age, creating more tolerance for shrinkage. Significant or circumferential burns may impact respiratory function or swallow, as well as the neurovascular systems. Facial burn rehabilitation is of great importance in the whole process of facial burn management, leading to better outcomes of facial burns after decades of clinical experiences. With the development of rehabilitative theory and techniques, facial burn rehabilitation nowadays should include updated content and advanced methods, and a comprehensive rehabilitation plan is necessary to enhance the quality of facial burn management. Initial rehabilitation before maturation of scars: combination of silicone gel with pressure therapy The combined intervention strategy of pressure therapy and silicone gel. The combination of silicone gel with pressure therapy has been shown to be more effective in providing benefits to the scar maturation outcome. It is also recommended by the ISBI Practice Guidelines Committee that all extensive burn hypertrophic scars should receive pressure therapy with silicone therapy as the first line of treatment. Since the facial contour is complicated with individualised convex and concave surfaces, the combined pressure therapy with silicone gel for facial hypertrophic scars needs a more customised intervention strategy. The 3D-printed transparent facemask with silicone linings is a promising solution for the effective application of the combined therapy. It has been used in our patients with favourable clinical results. But the patients need to maintain the treatment for at least half a year, until the maturation of the hypertrophic scars to achieve a stable clinical outcome. Scar massage Massage can increase the pliability of scarred skin, reduce pain,
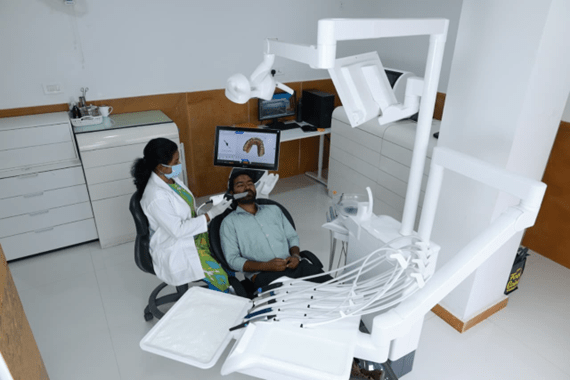
Comprehensive Dental Rehabilitation – Full Mouth Restoration (Case Presentation)
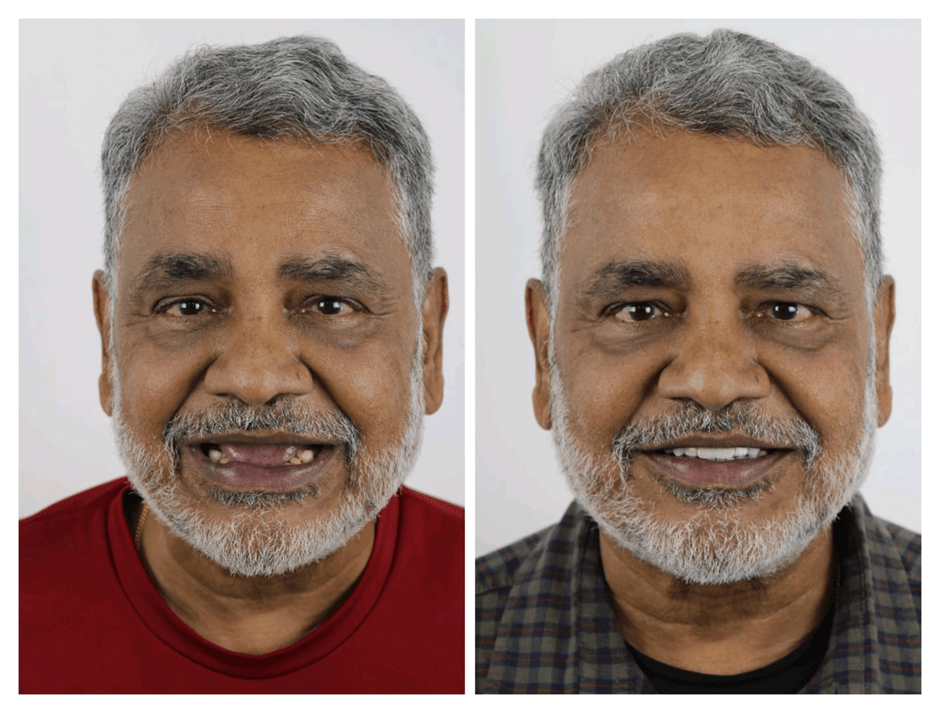
Full mouth rehabilitation, also known as full mouth reconstruction or restoration, is a comprehensive dental treatment that involves restoring the entire mouth to optimal health, function, and aesthetics. It encompasses various aspects to restore the patient’s functionality and aesthetics. 1. Comprehensive approach: Involves multiple procedures. 2. Restoring function: Improving chewing, occlusion, and speaking. 3. Aesthetic improvement: Enhancing the appearance and smile pattern, 4. Pain relief: reducing the discomfort. VARIOUS METHODS OF RESTORING A FULL MOUTH 1. Dental implants 2. Crowns 3. Bridges 4. Veneers 5. Orthodontics 6. Periodontal therapy Full mouth rehabilitation is a personalized treatment plan designed for each patient’s unique needs. CASE HISTORY Patient has no relevant medical history, controlled diabetes, under medication. 73-year-old male patient with a chief complaint of a badly done upper prosthesis (anterior teeth) elsewhere Lower arch presented with a few mobile teeth and chipped crowns INTRAORAL EXAMINATION TREATMENT PLAN FULL MOUTH REHABILITATION 1. Upper implant-supported prosthesis 2. Lower rehabilitation using a fixed partial denture UPPER IMPLANT SUPPORTED PROSTHESIS LOWER REHABILITATION USING A FIXED PARTIAL DENTURE The treatment plan is executed in 2 phases PHASE 1 PHASE 2 FABRICATION OF 4 UPPER IMPLANT-SUPPORTED PROSTHESIS Steps Impression coping in dental implants is a crucial step in the fabrication of implant-supported restorations. Purpose 1. Accurate transfer: Transferring the implant position to a working model. 2. Restoration fabrication: Creating precise implant-supported crowns or prosthesis. The technique we used is the open tray technique, which is a method to capture the precise position and orientation of dental implants. Key Steps 1. Impression coping placement: An impression coping is attached to the implant or abutment. 2. Tray preparation: A custom tray with an open top is used. 3. Impression material injection: Impression material is injected around the coping. 4. Tray removal: The tray is removed, and the coping remains in the impression. Impression coping in dental implants requires expertise and attention to detail. Impression coping Open tray technique 2. jig trial A jig trial is a verification process in dental implantology where a precise replica or jig of the planned prosthesis is used to check the accuracy of implant placement and the fit of the prosthesis on the implants. Procedure 1. Jig fabrication: A verification jig is created based on the planned restoration. 2. Trial fitting: The jig is tried on the implants to verify accuracy. Purpose Confirm implant positions match the planned restoration. 2. Assess fit: Evaluate the fit of the prosthesis on the implants. 3. Bite registration Bite registration is a dental procedure that records the relationship between the upper and lower teeth, capturing the precise occlusal relationship. Occlusal relationship: Records how the upper and lower teeth interact. Accurate capture: Ensures precise bite registration. This procedure is essential for full mouth dental rehabilitation to record the vertical ,horizontal relationships of the upper and lower jaws. 4. Denture trial To determine the position and vertical dimension of the final prosthesis A denture trial in full mouth rehabilitation is an inevitable step where a trial denture is placed in the patient’s mouth to: 1. Assess the denture’s fit and comfort. 2 . Evaluate the appearance and smile. 3. Check the denture’s function and bite. It allows for necessary adjustments before final cementation and Ensures patient satisfaction with the denture’s appearance and function. 5. Metal framework trial It will ensure the framework fits accurately on the implants and passively on the implants also evaluate the framework’s relationship with opposite teeth It minimizes the risk of implant failure or prosthesis malfunction and ensures optimal function and aesthetics. The metal framework trial is essential for achieving a successful implant-supported prosthesis. 6. Bisque trial A bisque trial in full mouth rehabilitation is a step where a trial prosthesis, typically made of ceramic or porcelain, is placed in the patient’s mouth to evaluate aesthetics, fit, and occlusion It allows necessary adjustments before finalization, also patient satisfaction with aesthetics and function. 7. Final cementation Intraoral and extraoral images of before and after
A Comprehensive Analysis of Hemangiomas of the Face

Introduction Vascular lesions, more commonly known as Haemangioma, are anomalies involving an abnormal growth of blood vessels. These hemangiomas of the face can range from benign conditions, such as Hemangiomas and vascular malformations, to more complex and potentially life-threatening lesions, like Arteriovenous Malformations (AVMs). In the face and neck, hemangiomas of the face can cause functional impairment, significant cosmetic deformities, and psychological implications. They become a reason of concern, particularly when they affect critical areas such as the airway, face, or eyes. Vascular lesions may occur in both children and adults, with some types being congenital and others acquired later in life. Classification Vascular lesions, including hemangiomas of the face, are classified into vascular malformations and vascular tumours: Vascular malformations –These are lesions arising from abnormal development of blood vessels during embryogenesis. Unlike tumours, they do not exhibit rapid growth but instead grow proportionally with the individual. Different types of vascular malformations include arteriovenous malformations, capillary malformations, venous malformations, and lymphatic malformations. Arteriovenous malformations are high-flow with a characteristic sound called bruit and are pulsatile in nature. Venous malformations are low-flow, bluish masses and often contain calcified blood clots called phleboliths. Lymphatic malformations, like hemangiomas of the face, may also present as soft, compressible lesions that can cause swelling and deformity in affected regions. Vascular tumours –Vascular tumours are characterised by an abnormal proliferation of blood vessels. These include hemangiomas of the face, which are the most common vascular tumours in infants and children. b. Haemangiomas:Benign tumours of endothelial cells that typically present in infancy. They show rapid growth followed by gradual involution or shrinkage over time. Depending on the location, they may cause cosmetic issues, airway obstruction, or visual impairment. Involuted haemangioma lesions of the face before and after surgical excision Clinical features of vascular lesions Cosmetic deformities- Port-wine stains or haemangiomas can cause significant cosmetic concerns. Port wine stain Patients with hemangiomas of the face or other visible vascular lesions may experience psychological distress, social stigma, and low self-esteem. In many cases, haemangiomas are asymptomatic. However, in critical areas, they can cause vision problems if located near the eyes, airway obstruction if on the neck near the respiratory tract, and functional impairment due to facial distortion or restricted movement. AV malformations may cause pain if located in deeper tissues, while vascular malformations may cause swelling that presents as soft, compressible, or spongy masses. Hemangiomas of the face can also lead to bleeding — high-flow lesions like AV malformations are prone to spontaneous or trauma-related bleeding, while low-flow malformations such as venous malformations may bleed if severely injured or ulcerated. Diagnosis of vascular lesions Clinical examination with a detailed history is essential for identifying the type, location, and extent of the lesion Imaging studies, such as ultrasound,d helps evaluate the depth and blood flow MRI or MRA provides detailed information about these signs and extent of the lesion and the blood supply to the lesion Biopsy is done in cases where the diagnosis is unclear MRI of the face showing vascular malformation Treatment of vascular lesions Observation-Many vascular malformations, particularly small and asymptomatic ones, simply require monitoring over time. Hemangiomas of the face, particularly in infants, often undergo involution without treatment Medical treatment- Propranolol and corticosteroid therapy is used to reduce the size and vascularity of the hemangioma by inhibiting new blood vessel formation and promoting involution. They also promote fibrosis of the lesion. Sclerotherapy involves multiple injections at regular intervals or until the lesion regresses in size either prior to or post surgical excision. Sometimes it is the only treatment modality followed for lesions and good results are seen Surgical treatment- Debulking of the lesion refers to removal of part of the lesion, usually done when the lesion is very large or is close to a critical structure or when complete excision of the lesion is not possible in one surgery. Surgical excision of the lesion refers to complete removal of small to moderately sized lesions In some hemangiomas of the face, excision may be considered for residual lesions that persist after involution. Embolization- For high-flow lesions like AVMs, embolization involves introducing substances into the blood vessels to block/reduce the blood flow to the abnormal vascular channels. This then reduces the size and vascularity of the malformation. This procedure is usually done by an interventional radiologist and most often in conjunction with surgical excision of large tumours. Laser therapy- Pulsed dye lasers are particularly effective for superficial capillary malformations such as port wine stain and help reduce redness and the appearance of the lesion Complications Bleeding, particularly in high-flow lesions Infection Functional impairment when lichens are located near vital structures it can lead to breathing difficulties, visual disturbances or swallowing problems Cosmetic deformities, visible lesions Prognosis Most vascular lesions, if managed appropriately, have a good prognosis, but cosmetic outcomes vary according to the lesion.
