The most effective treatment for obstructive sleep apnea (OSA) is continuous positive airway pressure (CPAP). But more than 50% of people cannot handle this procedure in the long term. As a result, several surgical techniques have been put forth; however, maxillomandibular advancement (MMA), which has an 86% success rate, has been demonstrated to be the most successful alternative for treating OSA in some individuals.
Maxillomandibular advancement (MMA), sometimes referred to as bimaxillary advancement surgery or double jaw surgery, is the primary type of bone surgery used for treating OSA. When upper and lower jars are small, it causes decreased airway diameter, leading to obstruction of airflow while sleeping. MMA expands these jaws, which encircle the airway, enlarging the entire airway, including the nasal, pharyngeal, and also airway below the pharynx.
INDICATIONS:
- Lack of compliance or intolerance to CPAP treatment.
- Serious side effects from CPAP treatment.
- Patient rejects all other choices (CPAP, oral appliance) and requests surgery.
- The patient’s anatomy makes surgery extremely advantageous.
PREOPERATIVE ASSESSMENT FOR MMA:
A detailed medical is taken, a physical examination is performed, polysomnography to diagnose and confirm OSA is done, and a questionnaire containing sleep-related questions is given, to score sleep (to assess the severity). Preoperative records are taken and facial and oral imaging are done to plan the treatment.
- Medical, family, and personal history: regarding smoking, alcohol, medications, etc.
- Sleep history: it includes
- History regarding likelihood of OSA: snoring (loudness, duration, etc.), breathlessness (choking, gasping, self-waking episodes)
- History regarding sleep architecture and hygiene: sleep onset/offset, difficulty in sleeping, sleep position (on back, lateral)
- History regarding consequences of OSA: weight gain, headaches, daytime tiredness, work issues.
- Physical examination: weight, height, the circumference of the neck, nasal Oral examination of position and size of the tongue, tonsil, palate, the position of jaws, occlusion (teeth position while biting)
- Upper airway assessment: A flexible digital camera will be used to inspect your upper airway while you lie back on the examination chair. By examining the upper airway and back of the throat, it is possible to more accurately assess the blockage locations that cause OSA.
PREOPERATIVE RECORDS AND IMAGING:
Before starting the procedure, dental impressions and preoperative photos are taken, dental models are prepared, and dental x-rays are taken, such as lateral cephalograms and cone beam computed tomography (CBCT).
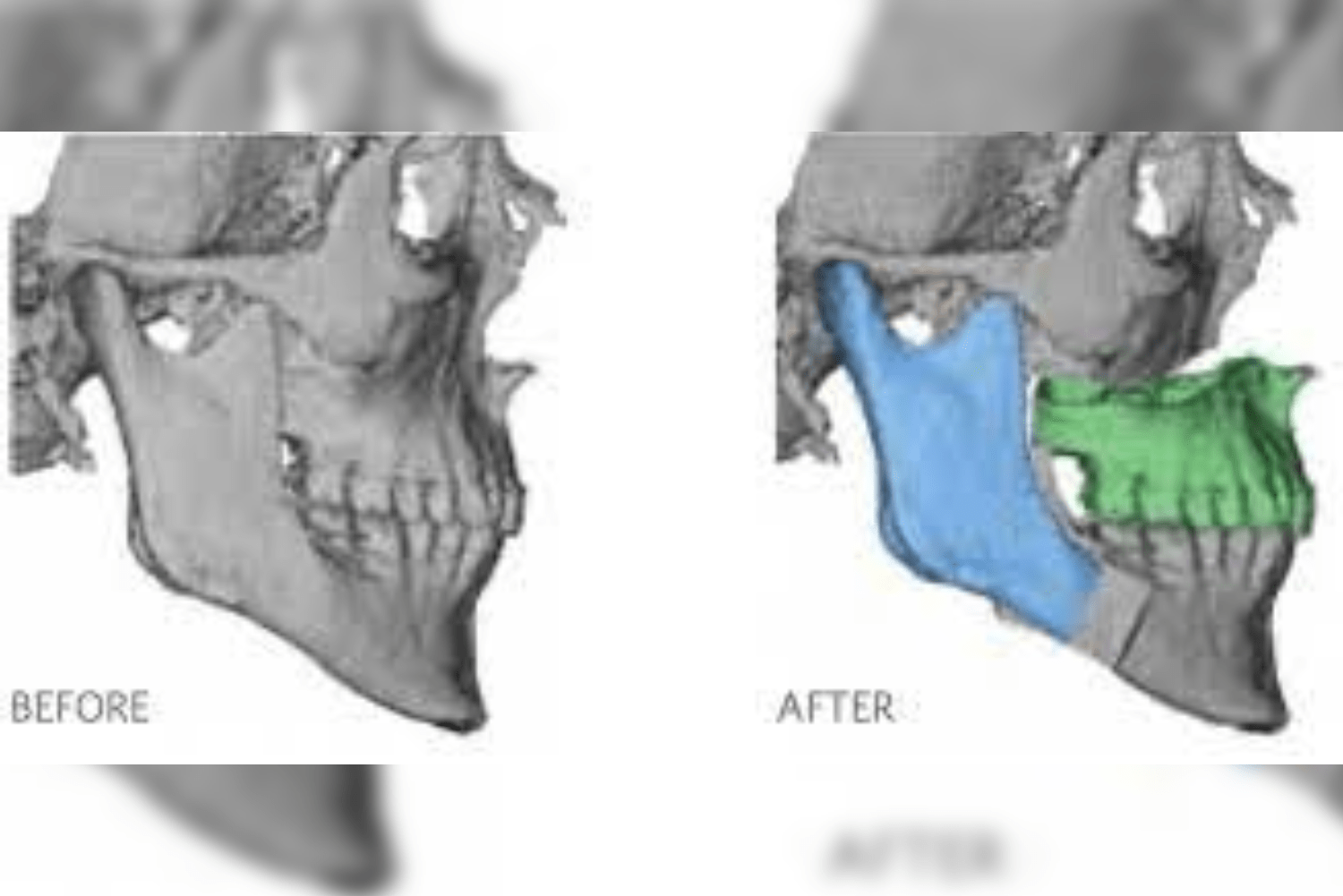
SURGICAL PLANNING USING DIGITAL 3D MODELS:
An accurate digital three-dimensional (3D) model of your skull and jaws will be created using dental models, CT scan photos, and CBCT. This graphical 3D representation produces a highly accurate depiction of the relationship between upper and lower jaws. The motions of the jaws and the surgical bone cuts are accurately planned using this 3D virtual model. It also helps to mark the important structure, which can help during surgery. A 3D printer is used to design and construct dental splints. During the procedure, these splints help to position the jaws precisely where they should be in order to maintain the patient’s bite.
SURGICAL PROCEDURE:
Surgery is done in a general anesthesia setting. A pre-anesthetic evaluation is done before the procedure. The anesthesiologist will put the patient to sleep, and a breathing tube and urinary catheter are inserted.
Arch bars (teeth brace-like appliances) are placed on the upper and lower teeth to maintain teeth in position (tooth bite). A small incision is made on the inner aspect of the upper lip, and the upper jaw is exposed. The bone is cut and moved forward according to the 3D model. The jaw is secured in place with the help of titanium screws and miniplates. One more incision is made on the inner aspect of the lower lip to expose the lower jaw. The bone is cut and moved forward according to the 3D model and secured in place by titanium screws. After confirming the correct bone position and occlusion, the incisions are closed by suturing, and the breathing tube is removed.
Combination surgery along with MMA can also be done if required, such as septoplasty, adenectomy, and tonsillectomy
POST-OPERATIVE CARE:
After the surgery, when the patient wakes up, he/she will be transferred to the intensive care unit (ICU) for a day for closer monitoring. The next day they will be transferred to a regular room if the patient is stable and allowed to begin oral feeding and walking. Patient will be asked to practice drinking as demonstrated by the doctor and perform a nasal wash. Pain medications are given, and a postoperative CT scan is performed. Patient is advised to sleep in a later position and may be discharged on second day if no complications are seen.
FOLLOW-UP/OUTCOME ASSESSMENT:
The patient will be recalled at intervals of one week, three weeks, and six weeks after discharge. During this time, the physician will assess the healing of the wound, bite, and sensation in the face. Initially, a pureed diet is recommended, and by 6 weeks, the patient will be asked to start a soft diet.
Three months after the surgery, the jaws will be completely healed and can have a normal diet. Physiotherapy should be started to increase your ability to open your mouth. Tongue depressors are placed between teeth, and the number of tongue depressors is gradually increased day by day till 4 cm of mouth opening is achieved.
Six months after surgery, postoperative photographs and x-rays are taken, and patients need not visit the doctor unless any complications arise or any additional attention is required.
SIDE EFFECTS:
- Swelling seen in and around the mouth: application of ice, sleeping on an inclined plane, and walking can help reduce swelling.
- Numbness of lips, cheeks, and chin – usually it is temporary. Usually resolves on its own over some weeks to a few months.
- Bite changes are common and resolve on their own. Sometimes dentist intervention is required to resolve the problem.
- Nasal congestion due to blood clots
- Decreased mouth opening: Three months after surgery Physiotherapy can help to increase mouth opening.
- Pain is uncommon, but if it persists, then pain medication is given.
- Nausea and vomiting are common after recovering from anesthesia. It can be managed by anti-nausea medication
POSSIBLE COMPLICATIONS:
- Temporomandibular joint pain (jaw joint): due to forward positioning of jaws. Another surgery may be scheduled in case of long-standing discomfort.
- Necrosis of the palate: caused by damage to the blood vessels of the palate, causing compromised blood supply.
- Long standing numbness of face
- In rare cases, nonunion of bones due to impaired healing or infection
- Dental damage: unwanted movement of teeth, tooth discoloration, fracture of teeth can be noted. It can be corrected by the dentist.
- Infections around the screws and plates can develop. It can be prevented by antibiotic administration.
IMPORTANT CONSIDERATION FOR MMA SURGERIES:
- The first four to six weeks following surgery are the most difficult for recovery because of swelling, numbness in the lips and mouth, and dietary restrictions. It might take up to a year for numbness to go away.
- Weight loss is common post-surgery due to dietary restrictions.
- Facial appearance changes as jaws are moved forward.
CONCLUSION:
CPAP remains the standard treatment for OSA. However, MMA provides an alternative option for those who cannot tolerate CPAP. This technique is associated with potential complications and adverse effects. Hence, the doctor should discuss available treatment options first and then decide the suitable treatment for the benefit of the patient.