A dental emergency is a situation that requires immediate attention from a dentist to reduce severe pain, prevent further damage, or save a tooth. There are two categories of dental emergencies

A.Common dental emergencies
These are
1. Severe toothache: Intense pain or swelling in the tooth or surrounding area, or severe orofacial trauma
2. Trauma: Injury to the vital teeth, mouth, or gums
3. Knocked-out tooth: Tooth is completely avulsed from the socket
4. Broken or chipped tooth: Trauma to a tooth
5. Infection: acute apical abscess, irreversible pulpitis, or severe dental caries
Acute pain is generally time-limited and responsive to pharmacotherapy or direct intervention.
Examples of conditions known to cause chronic pain in a dental setting are
- Chronic periodontal /pulpal infection,
- Rampant tooth decay, or
- Dentinal hypersensitivity
The immediate attention to the cause is necessary when treating emergencies; these are
- Identification of the cause of pain.
- Use of non-pharmaceutical therapies in applicable cases.
- Patient education for pain relief measures.
- Prescribing the required medications for pain relief.
Procedures:
- Initial assessment and regular reassessment of pain.
- Pain screening and evaluation
- The dentist should assess pain intensity and quality (for example, pain character, frequency, location, duration), based on both patient self-reporting and clinical measurements.
- When assessing pain, the dental provider may perform a variety of clinical tests, such as heat response (GP stick), percussion sensitivity, palpation of the affected region, or, in some cases, it may be assessed with a dental handpiece.
- Education of patients and families when appropriate, regarding risks and benefits and limitations of chosen pain relief modalities. Education of patients and families about their roles in effective pain management, as well as the side effects of pain treatment.
NON-PHARMACEUTICAL THERAPIES FOR DENTAL PAIN:
- Endodontic access – where pulpitis exists, the dentist has deemed the tooth salvageable, and the patient desires to save the tooth, the dentist may access the tooth pulp and remove the major dental nerves to the tooth, usually under local anesthesia.
- Intermediate Restorative Material (IRM) – where pulpitis exists, but the dentist is unable to determine if it is reversible or irreversible, an IRM may be placed on the tooth with or without local anesthesia.
- Extraction – where pulpitis, necrosis/abscess, or severe periodontal disease is diagnosed, the dentist may extract the affected tooth to manage the patient’s pain.
- Anesthesia – one short-term pain management technique is through the delivery of anesthesia to the affected site. This is usually used in conjunction with another treatment modality.
- Temporomandibular joint manipulation – If pain is present in the TMJ, the dentist may either physically manipulate the TMJ or massage gently available muscles of mastication (temporalis, masseter, etc.). This may be combined with pharmaceutical therapy or may in itself, relieve the patient’s pain.
- Occlusal adjustment – If pain is present due to Bruxism or occlusal trauma, the dentist may adjust the occlusion with a dental handpiece for effective pain management.
- Denture adjustment – If pain is present in the edentulous patient, the dentist or dental assistant may adjust the patient’s denture, and the dentist may cauterize the ulcerated region of tissue affected by the ill-fitting denture (silver nitrate stick, etc.).
PHARMACEUTICAL THERAPIES FOR DENTAL PAIN
The most commonly prescribed drugs for dental pain in our hospital are
- Paracetamol 650 mg
- Ketorolac dispersible tablets 10mg
- Aceclofenac 100mg + paracetamol 325 mg combination
All the above-mentioned drugs are given through the oral route.
For children, the dosage is calculated according to body weight, and usually paracetamol is given through the oral route in the form of syrup. The maximum dosage of paracetamol per kg body wt. is 10-15mg/kg body weight. Based on the pain intensity, the syrup can be given 3-4 times daily. The paracetamol syrup is available in two concentrations: 125mg/5 ml and 250mg/5 ml.
The dosage of the oral medication is decided depending on the patient’s intensity of pain, severity of the condition, and the patient’s accompanying medical conditions.
B.On chair dental emergency
“On chair dental emergency” is a situation where a patient experiences a dental emergency while already undergoing dental treatment on the dental chair
Possible Scenarios
1. Sudden pain or discomfort: Patient experiences unexpected pain or discomfort during a procedure
2. Tooth fracture or breakage: Tooth breaks or fractures during treatment
3. Instrument breakage: Dental instrument breaks or gets stuck in the patient’s mouth
4. Allergic reaction: Patient has an allergic reaction to a medication or material used during treatment
The most common medical emergencies that can occur in a dental chair are
- Asthma
- Epileptic Seizures
- Anaphylactic Shock and Allergies
- Diabetes (hypoglycemia/hyperglycemia)
- Syncope
- Myocardial Infarction
- Choking due to airway obstruction by a foreign body
ASTHMA
Signs and Symptoms:
Wheezing when exhaling, coughing, and shortness of breath
Treatment Precautions:
• Make sure the patient has their medication with them at the time of the appointment
• For controlled asthmatics, LA with Epinephrine should be used judiciously; this is because the sulphite used as a preservative may bring about an allergic attack.
• Agree on a signal for distress with the patient before beginning treatment
• Avoid Aspirin or NSAIDS
Treatment:
• Have the patient signal you that they need their medication
• Have the patient administer their own medication (bronchodilators)
• Deriphyllin (i.v.) and Salbutamol inhaler are to be given
• Administer Oxygen if deemed necessary
EPILEPTIC SEIZURES
Signs and Symptoms:
• Patient may have a previous history of seizures
• Patient may recognize they are coming by a preceding “aura”
• Altered consciousness levels
• Muscle rigidity
• Convulsions
• Apnea (temporary absence or cessation of breathing)
• Cyanosis
Treatment Precautions:
• If the patient usually recognizes when seizures are about to happen, discuss a signal they can give about an impending seizure
• Make sure the patient has taken their medication that day
• Have Oxygen Ready
• Be prepared to remove the clamp, rubber dam in case of an episode of seizures.
Treatment:
• Place the patient on his side on the floor away from objects until the seizure subsides
• If the patient vomits, suction
• If seizure lasts longer than 5 minutes, call for Emergency Medical Services
• Administer Oxygen if deemed necessary
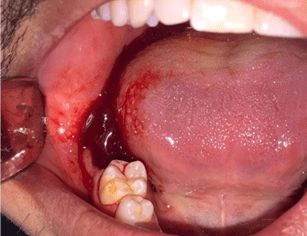
ANAPHYLACTIC SHOCK/ ALLERGIES
Signs and Symptoms:
• Respiratory distress, wheezing
• Airway obstruction
• Rapid, weak pulse
• Palpitations
• Swelling of lips or eyelids, eyelids may itch and tear
• Difficulty swallowing
• Nausea and vomiting
• Urticaria (hives)
Treatment Precautions:
• Always perform a complete medical history to reduce the likelihood of an allergen exposure
Treatment:
• Call EMS immediately
• Administer epinephrine
• If pulse present, elevate legs, give oxygen
• If no pulse or breathing, begin CPR
• If the patient vomits, suction
• Continue CPR or monitor vital signs until EMS arrives
DIABETES
Elevated glucose levels in blood and urine. Persons diagnosed with Diabetes may suffer from too high or too low blood sugar at times, depending on medications, food intake, illnesses, or stress.
Signs and Symptoms:
Hypoglycemia
Rapid onset –within minutes, Nervousness, Pallor, feeling Weak and dizzy, Hunger, nausea, Mental confusion, Lethargy, Decreased rate of breathing, Increased heart rate, Decrease in blood pressure, Seizures, Tingling sensation in feet/hands, Loss of consciousness.
Hyperglycemia
Slow Onset – hours or days, feeling Hot and dry, flushed malaise, Nausea and vomiting, Stupor, Drowsy, Irritability and Headache, Acetone odor, decreased blood pressure, increased heart rate
Treatment Precautions:
• Ensure the patient has eaten and has had their medication before the appointment
• Keep appointments short
• Have a sugar supplement on hand
Treatment:
• If conscious and able to swallow well, give a sugar supplement. Call for Emergency Medical Services if the patient doesn’t feel better in 15 minutes or becomes unconscious.
• If unconscious, call Emergency Medical Service immediately
SYNCOPE
Temporary loss of consciousness with inability to maintain postural control
Causes:
• Fear, pain, or stress
• Fatigue
• Overly warm environment
• Decreased blood flow to the brain, vasovagal event
Signs and Symptoms
• Restlessness
• Pallor
• Feeling “too warm”
• Cold and clammy skin
• Nausea, generally feeling unwell
• Breathing may be irregular
• Slow, feeble pulse
• Convulsive movements, twitching
• Loss of consciousness
Treatment:
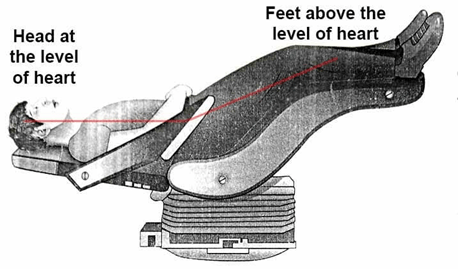
• Lay patient in a horizontal “head below feet” position
• Loosen tight clothing
• Monitor ABC’s (Airway, Breathing, and Circulation)
• Ask the patient to smell a cotton pledget soaked in spirit of ammonia (respiratory stimulant)
• Give Oxygen if required
• Call for emergency medical services if the patient does not recover within 10 minutes
MYOCARDIAL INFARCTION
Signs and symptoms
• Chest pain of pressure.
• Patients may also experience shortness of breath, fainting, nausea or vomiting, sweating, anxiety.
• Pain radiating to the left shoulder or lower jaw
Treatment:
• Call for emergency medical services immediately.
• Aspirin
• Oxygen
CHOKING
Foreign bodies may cause either mild or severe airway obstruction. A severe airway obstruction can progress to unconsciousness and cardiac arrest within minutes.
Signs and symptoms
Mild obstruction: Patient can answer questions, speak, cough, and breathe.
Severe obstruction: Inability to answer questions, dyspnoea, wheeze, silent cough, cyanosis, unconsciousness.
Management
Mild obstruction: Patient is encouraged to cough, continue to check for deterioration to an ineffective cough or relief of obstruction.
Severe obstruction: Patient has an ineffective cough; the Patient is given abdominal thrusts by Heimlich’s maneuver and back blows. Immediately start CPR if the patient is unconscious. Call for emergency medical services.
THE COMMON EMERGENCY MEDICINE SHOULD BE KEPT IN THE DENTAL CLINIC
1. Injection of Atropine for bradycardia
2. Injection Dopamine-vasostimulant used to treat low blood pressure, low heart rate, and cardiac arrest.
3. Injection Dobutamine-used short-term to treat cardiac decompensation due to weakened heart muscles, usually given after other cardiac medicines have been tried without success.
4 . Injection Deriphyllin– a combination of two bronchodilators, etophylline + theophylline, to treat asthma and COPD
5. Injection metolar-hypertensive emergency, angina, arrhythmia
6. Injection Heparin, an anticoagulant
7 Injection Avil-allergic conditions like hay fever, food allergy, drug rashes, skin allergy
8 Injection ondansetron-used to prevent nausea and vomiting
9. Injection metoprolol is used to reduce the risk of death from an acute heart attack
10. Injection of gentamycin to treat serious bacterial infections in many different parts of the body.
Injection Glycopyrolate-used is used as a preoperative medication to inhibit salivary gland and respiratory secretions
11. Adrenaline injection to treat a severe allergic reaction(anaphylaxis)in emergency conditions like anaphylactic shock.
12. Injection of ketorolac tromethamine-NSAIDs to relieve severe pain.
13. Injection of sodium chloride, a source of electrolytes and water for hydration.
14. Injection pantoprazole for acid reflux and peptic ulcer.
15. Injection of tranexamic acid to control excessive bleeding during a dental procedure with hemophilia.
16. Injection of amikacin sulphate to treat serious bacterial infection.
17. Injections of Lasix to treat fluid retention, edema
18. Injection of ranitidine to treat various ulcers, like duodenal, gastric, and postoperative ulcers.
Injection of ephedrine for hypotension caused by anesthesia, allergic conditions, bronchial asthma, and nasal congestion.
19. Injection of phenytoin sodium for the treatment of epilepsy, seizures
20. Injection of calcium gluconate for the treatment of low-level calcium
21. Injection of potassium chloride for treating low levels of potassium
22. Injection Avil (pheniramine maleate ) is an antihistamine drug for the treatment of drug rashes, hay fever, food allergy, itching skin conditions, angioneurotic edema, and allergic conjunctivitis.
23 Injection aminophylline for the treatment of severe and life-threatening asthma, bronchitis, emphysema, and other lung diseases in a hospital setting up
