Oral Cancer Treatment
Oral cancer has the highest prevalence in India. It ranks as the third most common cancer in India, posing a significant public health problem. It’s the most common cancer in men and the third most common in women. A large proportion of oral cancers in India are linked to tobacco use, particularly smokeless forms like gutkha, betel quid, and areca nut. Early diagnosis and effective oral cancer treatment at Richardsons play a vital role in improving outcomes and saving lives.
The surgery for oral cancer will be aggressive in nature, as is the disease, due to its fast-spreading capability.
Surgery for oral cancer involves removing a large part of the tumour along with the surrounding organs involved. It may include removal of parts of the oral cavity, mandible, tongue, and buccal mucosa.
This leads to a significant compromise in the form and function of the face. Reconstruction in oral cancer patients is a vital component of comprehensive cancer care. The aim is to restore form and function—including speech, swallowing, mastication, and appearance—after tumour resection. It depends on the tumour size, location, expertise of the surgeon, and any comorbidities the patient may have. Comprehensive oral cancer treatment at Richardsons focuses on both life-saving surgery and advanced reconstructive care to ensure optimal recovery and quality of life.
The goal of the reconstruction is to:
- Restore speech, swallowing and mastication.
- Reconstruct bone and soft tissue defects.
- Maintain aesthetics and Facial symmetry.
- Enable dental rehabilitation
- Improve quality of life by reducing functional morbidity
Types of Defects and Reconstructive Options:
Each patient has unique challenges, and reconstruction is highly individualised based on the size and location of the cancer. As part of comprehensive oral cancer treatment at Richardsons, reconstruction is carefully planned to restore both function and appearance.
-
Tongue and floor of mouth cancer: Reconstruction is done using soft tissue flaps such as the radial forearm or anterolateral thigh flap, which aids in preserving mobility and speech function.
-
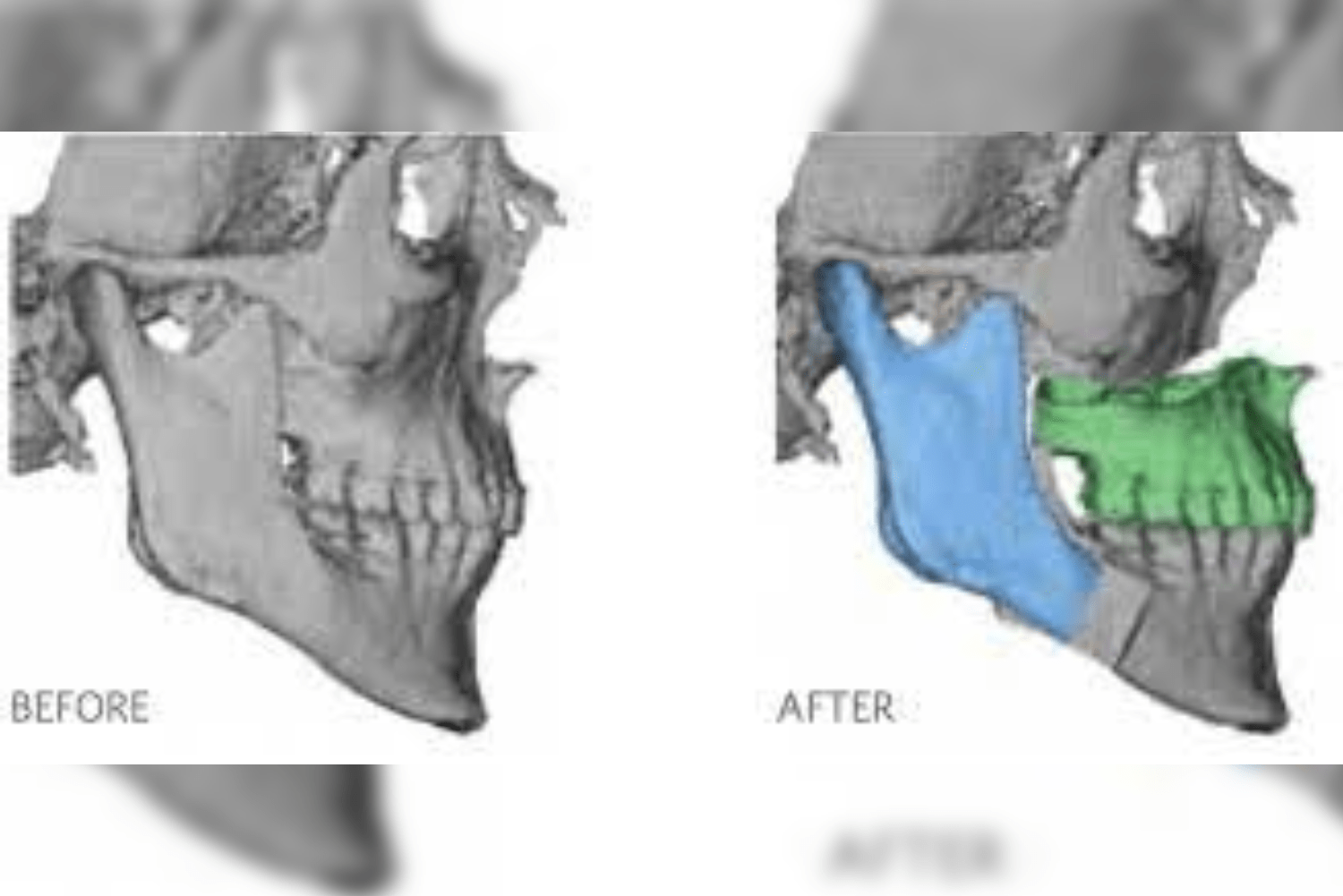
Mandibular jaw bone defects: These often require reconstruction using bone. A fibula free flap, and at times iliac bone or rib graft, is used to create structural integrity and allow for future placement of dental implants.
-
Buccal mucosa or lip defects: These are restored using local flaps or soft tissue from other parts of the body. Local flaps like the nasolabial flap, tongue flap, and temporalis flap or distant flaps like PMMC flaps are used for closure.
-
Maxillary defects: These may need both soft tissue and bone to restore the midface. Iliac bone or scapular grafts are often used for bone reconstruction. Soft tissue flaps like the temporalis, nasolabial, and tongue flaps help close soft tissue defects. Zygomatic implants have paved the way to reconstruct maxillary defects with dental rehabilitation.
With a focus on function, aesthetics, and long-term recovery, oral cancer treatment at Richardsons ensures that reconstruction is tailored to each patient’s unique needs for the best possible outcomes.
Pre-requisites for Surgery
A thorough assessment of the patient is essential pre-operatively as part of comprehensive oral cancer treatment at Richardsons. This ensures optimal planning for both tumour removal and reconstruction:
-
CT, MRI, or PET CT is taken to evaluate whether the patient is cancer-free. This ensures there is no residual or recurrent tumour before proceeding with reconstructive surgery.
-
The patient should have completed radiation or chemotherapy at least 1 year prior to reconstructive surgery.
-
Nutritional status of the patient must be assessed.
-
The patient should be healthy enough to accept a flap from a distant site for reconstruction.
-
Medical optimisation is required. The patient should have manageable levels of comorbidities such as diabetes, hypertension, or thyroid disorders.
-
Cardiopulmonary fitness must be evaluated to ensure the patient can safely undergo surgery.
-
Airway assessment is necessary for intubation or tracheostomy planning.
-
Dental evaluation is needed for remaining dentition and occlusion.
-
Smoking and alcohol cessation is advised prior to surgery.
All these factors are carefully considered under the expert protocol followed in oral cancer treatment at Richardsons, ensuring safe and successful reconstructive outcomes.
Microvascular Free Flaps: The Gold Standard
In modern times, surgeons prefer microvascular free tissue transfer, which has become the gold standard in reconstruction. As part of advanced oral cancer treatment at Richardsons, this technique ensures both precision and long-term functional recovery.
The tissue transplant is done along with its own blood supply from the arm, leg, or back, and it is reconnected to the vessels in the neck. This is performed under a microscope using loupes and suture material thinner than a hair strand. The vessels are attached seamlessly, without any leakage of blood.
These tissues or flaps may include skin, muscle, and bone, depending on the area that needs to be reconstructed. One of the most versatile options is the free fibula flap, which can provide up to 25 cm of bone for jaw reconstruction and can accommodate dental implants. This level of precision and expertise makes oral cancer treatment at Richardsons a trusted choice for patients requiring complex reconstructions.
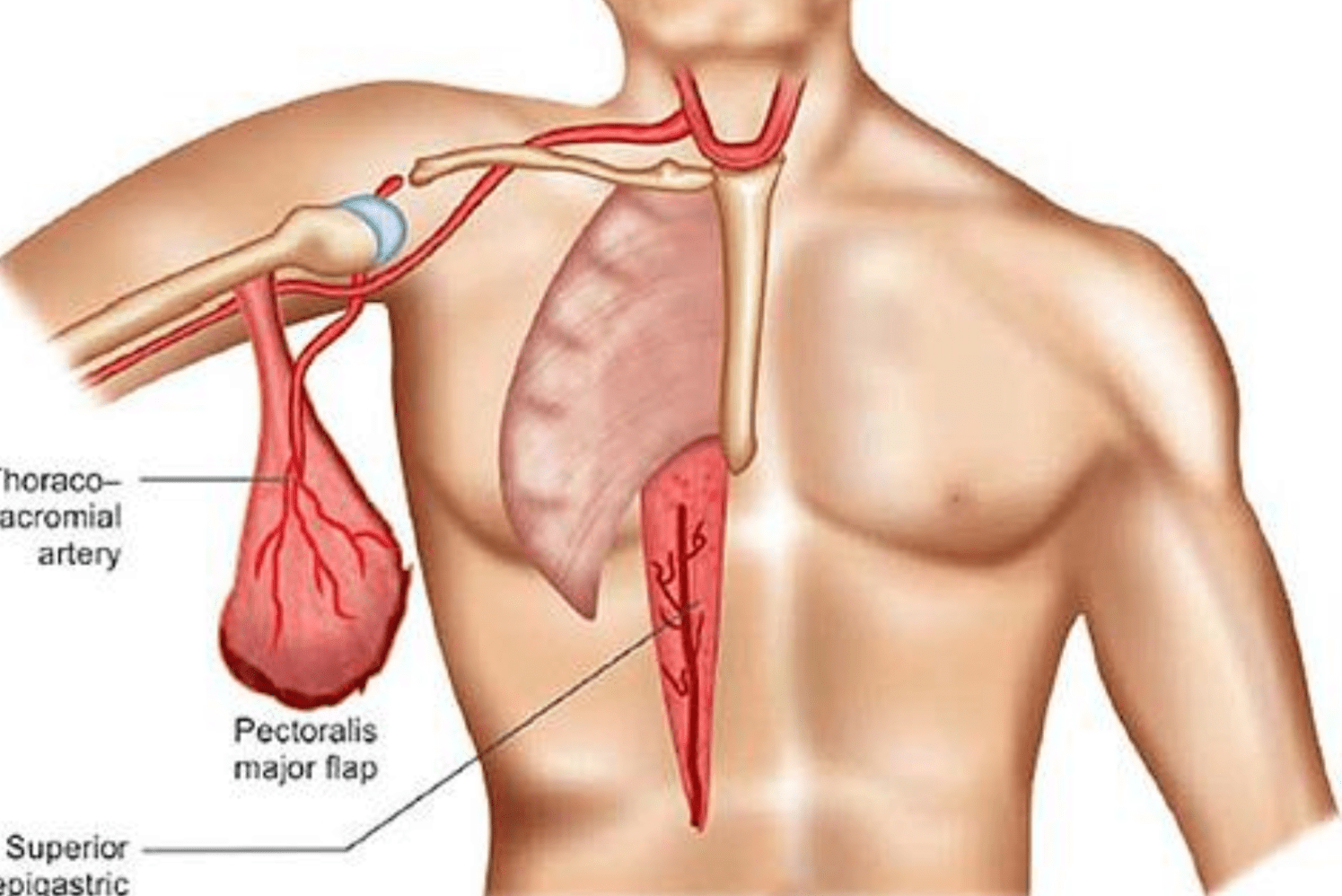
Reconstruction Using the PMMC Flap for Cases with Zero to Minimal Mouth Opening
Oral cancer, particularly squamous cell carcinoma, requires a combination of surgical resection, chemotherapy, and radiation therapy. As part of comprehensive oral cancer treatment at Richardsons, these modalities are tailored to ensure maximum disease control. However, they often lead to complications such as trismus or restricted mouth opening, even after the patient is disease-free. This severely affects the patient’s quality of life.
In advanced cases where fibrosis and osteoradionecrosis involve the mandible, segmental resection becomes necessary. In such cases, reconstruction is not optional but essential. One of the most reliable and cost-effective solutions in resource-limited settings is the pectoralis major myocutaneous flap (PMMC flap). This flap provides dependable tissue coverage and has been successfully used in many cases managed under oral cancer treatment at Richardsons, especially when microvascular reconstruction is not feasible.
Understanding Trismus Post-Radiation
Trismus, or restricted mouth opening, is a result of:
-
Radiation-induced fibrosis of the mastication muscles
-
Post-surgical scarring or fibrotic bands
-
Osteoradionecrosis of the mandible
Patients often experience:
-
Difficulty in food consumption
-
Difficulty in maintaining oral hygiene
-
Poor nutrition and weight loss
-
Slurred speech and, in severe cases, a compromised airway
When conservative measures like physiotherapy fail, surgical intervention becomes inevitable. As part of holistic oral cancer treatment at Richardsons, trismus is addressed with both rehabilitative and surgical strategies to restore oral function and improve quality of life.
Surgical Approach: Mandibular Resection
This procedure is indicated when there is:
-
Extensive fibrosis of the mastication muscles
-
Osteoradionecrosis of jaws
-
Worsening of trismus despite physiotherapy
-
A non-functional jaw interfering with daily activities
As part of advanced oral cancer treatment at Richardsons, mandibular resection is performed to restore essential functions and improve quality of life.
Procedure:
-
Segmental or marginal mandibulectomy is done depending on the extent of bone involvement
-
Debridement of necrotising tissue
-
Adequate release of trismus and restoration of mouth opening
Reconstruction Using PMMC Flap
This remains a workhorse flap in head and neck reconstruction, especially in resource-limited settings where microvascular free flap options are not feasible. The PMMC flap is a trusted choice in oral cancer treatment at Richardsons when immediate, functional reconstruction is needed.
Why PMMC?
-
Reliable vascularity through the thoracoacromial artery
-
Provides both skin and muscle bulk
-
Covers intraoral and external defects
-
Does not require microvascular anastomosis
-
Shorter operative time and lower technical demands
-
Low failure rates
Used extensively in oral cancer treatment at Richardsons, the PMMC flap offers a solid balance of reliability and function for patients who are not candidates for free flap surgery.
Flap Design:
-
A skin paddle over the pectoralis major muscle is included
-
The flap is tunnelled through the neck to cover defects of the neck and mandible
-
It provides support for mandibular contour
-
Can be combined with a titanium reconstruction plate to maintain mandibular continuity
Patient Counselling
Before surgery, patients undergoing oral cancer treatment at Richardsons are fully informed about expected outcomes, surgical risks, donor site morbidity, and the importance of postoperative rehabilitation. Consent is taken accordingly.
Postoperative Care and Rehabilitation
-
Wound care at recipient and donor sites with daily evaluations
-
Antibiotic management with high doses to prevent infection, especially in immunocompromised or nutritionally deficient patients
-
Early physiotherapy to initiate mouth-opening exercises and regain strength, flexibility, and mobility of jaw and neck muscles
-
Long-term physiotherapy is advised for sustained jaw mobility
-
Nutritional support via Ryle’s tube, gradually transitioning to oral feeding
-
Prosthodontic rehabilitation is considered feasible in the long term
Part of holistic oral cancer treatment at Richardsons, this comprehensive care approach ensures not only surgical success but also long-term functional recovery.
Note:
Mandible resection and reconstruction using a PMMC flap offer a functional and aesthetic solution to patients. While highly successful in treating intractable trismus post-radiation, the PMMC flap alone does not support dental rehabilitation. A second surgery with a bone graft or flap is required for dental implant placement.